Beta-lactamases are enzymes secreted by both Gram positive and Gram negative bacteria, and which have the ability to hydrolyze (breakdown) beta-lactam antibiotics. Beta-lactamases are responsible for bacterial resistance to broad class of-beta-lactam antibiotics, including the penicillins, cephalosporins and carbapenems. They provide antibiotic resistance in pathogenic bacteria by breaking the antibiotic structure, thereby leaving a molecule that is devoid of antimicrobial activity. Beta-lactamases are the most important cause of bacterial resistance to the beta-lactam antibiotics.
There are several groups and classes of beta-lactamases that result in antibiotic resistance. The beta-lactamases may be classified based on their preferential antibiotic target. For example, penicillinases, cephalosporinases, and carbapenemases are beta-lactamases that hydrolyze the penicillins, cephalosporins and carbapenems respectively. Beta-lactam antibiotics are antibiotics or classes of antibiotics that contain beta-lactam ring (a four-atom ring) as their main functional group.
The beta-lactamase enzymes breaks open this four-atom ring of the antibiotic; and in doing so, they deactivate the antibiotic and make it less efficacious in killing or inhibiting the growth of pathogenic bacteria in vivo or in vitro. Beta-lactam antibiotics are the cornerstone of our antibiotic armamentarium or therapy; and their mechanism of action is based on inhibition of bacterial cell wall synthesis. Beta-lactam antibiotics particularly the penicillins were the first group or class of antibiotics to be introduced into clinical medicine for the treatment of bacterial related infections including those caused by Gram positive and Gram negative bacteria.
Despite the potent antimicrobial activity of the beta-lactam antibiotics, bacteria (inclusive of Gram positive and Gram negative bacteria) have developed novel ways with which they evade the antimicrobial onslaught of the beta-lactams. One of the ways via which pathogenic bacteria resist antimicrobial action is to produce extracellular enzymes such as beta-lactamase enzymes – that deactivates the antibiotic meant to suppress their disease-causing ability in a host. There are several mechanisms through which microbes resist antimicrobial onslaught, but the production of beta-lactamase enzymes by microbes is one of the many ways via which pathogenic bacteria can make a particular antibiotic inefficacious for treatment.
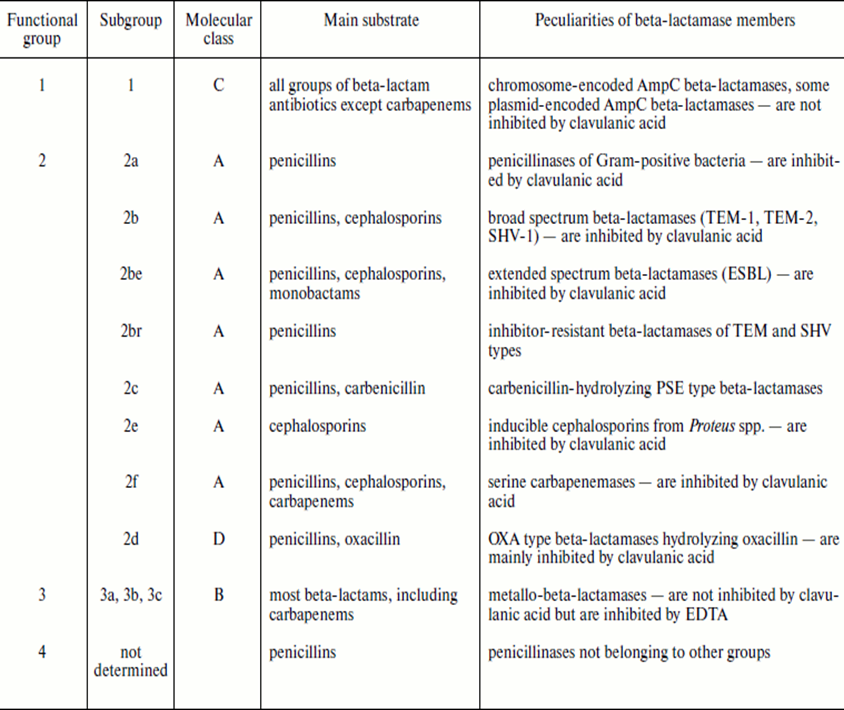
Beta-lactamase enzyme is one category of enzymes or drug resistance mechanisms put forward by microbes in the face of antimicrobial onslaught. Today, there are plethora of newer beta-lactamases including the extended spectrum beta-lactamases (ESBLs) and metallo beta-lactamases (MBLs) that defy the potent antimicrobial onslaught of novel beta-lactam antibiotics such as the cephalosporins and the carbapenems respectively. There is a functional and molecular classification of beta-lactamases; and these classifications are usually based on the amino acid sequences of the enzymes and on the type of substrates (antibiotics) that they have stronger affinity for (Table 1).
Table 1. Classification of Beta-Lactamase enzymes
References
Arora D.R (2004). Quality assurance in microbiology. Indian J Med Microbiol, 22:81-86.
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Axelsen P.H (2002). Essentials of antimicrobial pharmacology. Humana Press, Totowa, New Jersey, USA. Al-Jasser A.M (2006). Extended – Spectrum Beta – Lactamases (ESBLs): A Global Problem. Kuwait Medical Journal, 38(3):171-185.
Bisht R., Katiyar A., Singh R and Mittal P (2009). Antibiotic Resistance – A Global Issue of Concern. Asian Journal of Pharmaceutical and Clinical Research, 2 (2):34-39.
Block S.S (2001). Disinfection, sterilization and preservation. 5th edition. Lippincott Williams & Wilkins, Philadelphia and London.
Cars O and Nordberg P (2005). Antibiotic resistance: The faceless threat. International Journal of Risk & Safety in Medicine, 17 (3/4): 103-110.
Carson C.F., Hammer K.A and Riley T.V (2006). Malaleuca alternifolia (Tea Tree) oil: A Review of Antimicrobial and other Medicinal Properties. Clinical Microbiology Review, 19(1):50-62.
Cowan M.M (1999). Plant products as antimicrobial agents. Clinical Microbiology Reviews., 564-582.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA.
Ejikeugwu Chika, Ikegbunam Moses, Ugwu Chigozie, Eze Peter, Iroha Ifeanyichukwu, and Esimone Charles (2013). Phenotypic Detection of Klebsiella pneumoniae Strains – Producing Extended Spectrum β-Lactamase (ESBL) Enzymes. Scholars Academic Journal of Biosciences. 1(1):20-23.
Ejikeugwu Chika, Iroha Ifeanyichukwu, Adikwu Michael and Esimone Charles (2013). Susceptibility and Detection of Extended Spectrum β-Lactamase Enzymes from Otitis Media Pathogens. American Journal of Infectious Diseases. 9(1):24-29.
Ejikeugwu Chika, Iroha Ifeanyichukwu, Adikwu Michael and Esimone Charles (2013). Susceptibility and Detection of Extended Spectrum β-Lactamase Enzymes from Otitis Media Pathogens. American Journal of Infectious Diseases. 9(1):24-29.
Finch R.G, Greenwood D, Norrby R and Whitley R (2002). Antibiotic and chemotherapy, 8th edition. Churchill Livingstone, London and Edinburg.
Joslyn, L. J. (2000). Sterilization by Heat. In S. S. Block (Ed.), Disinfection, Sterilization, and Preservation (5th ed., pp. 695-728). Philadelphia, USA: Lippincott Williams and Wilkins.
Lai P.K and Roy J (2004). Antimicrobial and chemopreventive properties of herbs and spices. Curr. Med. Chem, 11 (11): 1451–1460.
Livermore D.M (2004). The need for new antibiotics. Clinical Microbiology & Infection, 4(10): 1-9.
Mascaretti O.A (2003). Bacteria versus antibacterial agents: An integrated approach. Washington: ASM Press.
Nally J.D (Ed.) (2007). Good manufacturing practices for pharmaceuticals. Sixth edition. Informa Healthcare USA, Inc, New York.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.