McFarland Turbidity Standard is an important technique performed in the microbiology laboratory especially when carrying out antimicrobial susceptibility studies. It is a turbid solution that contains a mixture of barium salt, distilled water and tetraoxosulphate (VI) acid (H2SO4). McFarland turbidity standard is used to compare and balance the turbidity of both the test and control microorganisms in the microbiology laboratory prior to microbiological analysis. This technique is important because it allows you to work with a defined concentration of the test or control organisms while removing all possibility of working with a high amount of the organism fro culture or other bacteriological purposes.
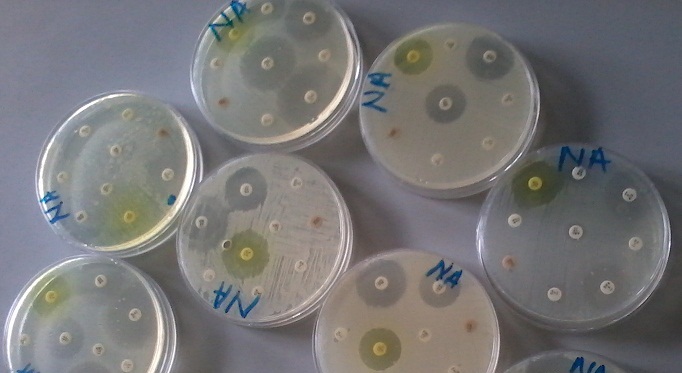
McFarland turbidity standard allows the scientist to work with the correct amount of the test or control organism in order to get a confluent growth on the culture media plate. McFarland turbidity standard is used to adjust the turbidity of the test inoculums/bacterium for the antimicrobial susceptibility test. The essence is to ensure that the researcher is working with the right number of organisms (in colony forming units, CFUs), and that the problem of “inoculums size”which might affect the susceptibility test (a process called inoculums effect) is well taken care of.
Already prepared McFarland turbidity standards are commercially available. Nevertheless, it can also be prepared traditionally in the laboratory. A typical example of McFarland turbidity standards used in the microbiology laboratory for antibiogram studies is 0.5 McFarland turbidity standard. A turbidity of 0.5 McFarland standards is approximately equal to 1.5 x 108CFU/ml of the bacterial suspension.
0.5 McFarland turbidity standard may be prepared as follows:
- Pour 0.6-ml of a 1% (10 g/L) solution of barium chloride dehydrate (BaCl2.2H2O) into a 100-ml measuring cylinder.
- Fill the measuring cylinder to 100-ml by adding 1% (10 ml/L) tetraoxosulphate (VI) acid (H2SO4) to the BaCl2.2H2O solution.
- Shake the mixture properly and aliquot into test tubes equivalent/identical to those used to prepare the inoculums/test organisms’ suspension.
- Seal the tubes properly to prevent evaporation.
- Store in the dark at room temperature. A properly stored aliquot can last for 6 months provided it is air tight to prevent evaporation.
Alternatively, 0.5 McFarland turbidity standards can be prepared as follows:
- Add 1 ml ofconcentrated H2SO4 to 99 ml of distilled water in a conical flask or beaker and mix well. In this way, a 1 % v/v solution of H2SO4 is prepared.
- Dissolve 0.5 g of dihydrate barium Chloride salt (BaCl2.2H2O) in 50 ml of distilled water. In this way a 1 % w/v of BaCl2 is prepared.
- Add 0.6 ml of BaCl2 solution to 99.4 ml of H2SO4 solution to make up to 100 ml.
- Mix the solution well. This is the stock solution of the 0.5 McFarland turbidity standards.
- Transfer about 2-3 ml of the solution into capped tubes and store at room temperature until use.
Note:
Acid should always be added to water and not the other way round. This is the best practice and it saves you from acid attack.
v/v = volume per volume
w/v = weight per volume
- The accuracy of the prepared 0.5 McFarland turbidity standard may be verified by adjusting the suspension of a control organism such as K. pneumoniae ATCC 700603 to the same turbidity standard prepared. The organism should be serially diluted at 10 fold dilutions and then plated. Plate counts should be performed, and the counted bacteria should read 108 CFU/ml. on the other hand, a spectrophotometer can be used to determine turbidity standards accuracy by measuring the absorbance of the solution. 0.5. McFarland turbidity standards should be read optical density (OD) value of 0.08-0.1 at a wavelength of 625 nm.
NOTE: Normal saline is prepared by dissolving 8.5 g of NaCl in 1 liter (1000-ml) of distilled water. The mixture can be autoclaved or filtered using membrane filters. Resultant solution is capped and stored at room temperature.
To match a test organism to the 0.5 McFarland turbidity standards: To prepare a McFarland standard against which a test inocula will be compared, sterile your inoculate loop over a Bunsen burner flame until it is red hot. Allow the loop to cool for about 30 seconds. Then, prepare the suspension of the test organism (s) or inocula by homogenizing several colonies of the inocula (preferably from an overnight culture plate) into sterile normal saline in a test tube (equivalent to the 0.5 McFarland standard turbidity solutions in a separate test tube).
Adjust the turbidity of each suspension visually to the 0.5 McFarland turbidity standards. After this preparation and the suspension is too light (i.e. has not matched the 0.5 McFarland turbidity standards solution in the other tube), add more colonies of the test organism to the tube (ensuring to sterilize your inoculating loop in the process).
But if the prepared suspension of the test organism(s) is too dense (i.e. thicker or more turbid) than the 0.5 McFarland turbidity standards, dilute the test organism suspension with normal saline until you have reached a turbidity that is comparable to the 0.5 McFarland turbidity standards solution in the other test tube (Figure 1). Now you can work with your test organism. It is noteworthy that matching this turbidity (i.e. 0.5 McFarland turbidity standards) with the test organism provides a bacterial inoculum concentration of 1.5 × 108 CFU/mL.
The McFarland turbidity standard indicates the correct turbidity of the test bacterium that is required for carrying out the testing or microbiological analysis (e.g. antimicrobial susceptibility testing). McFarland turbidity standard gives the researcher the appropriate concentration of the organism required for the analysis.

The tube on the right hand side is the McFarland standard while the tube on the left hand side is the test suspension. It the test suspension appears too dense when compared to the McFarland standard, it is required that you dilute the test suspension aseptically with the addition of broth or normal saline so that both the test suspension and the McFarland standard will have the same turbidity.
And if the test suspension is too light, aseptically inoculate the test suspension with the test organism from a pure culture plate or re-incubate the tube containing the test organism at the appropriate temperature for about 1 hour in order to increase bacterial growth.
Both the test suspension tube and the tube containing the McFarland standard should be placed in front of a paper as shown; and when it is more difficult to see the lines on the paper, then the test suspension is too dense and vice versa. You must see through the test solution to get the appropriate concentration of the organism when matched with the standard.
References
Arora D.R (2004). Quality assurance in microbiology. Indian J Med Microbiol, 22:81-86.
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Barenfanger J, Drakel C and Kacich (1999). Clinical and Financial Benefits of Rapid Bacterial Identification and Antimicrobial Susceptibility Testing. Journal of Clinical Microbiology, 37(5):1415-1418.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA.
Doern G, Brueggemannn A.B, Perla R, Daly D, Halkias D, Jones R.N, Saubolle M.A (1997). Multicenter laboratory evaluation of the bioMerieux Vitek antimicrobial susceptibility testing system with 11 antimicrobial agents versus members of the family Enterobacteriaceae and Pseudomonas aeruginosa. J Clin Microbiol, 35:2115–2119.
Doern G, Vautour R, Gaudet M, Levy B (1994). Clinical impact of rapid in vitro susceptibility testing and bacterial identification. J Clin Microbiol, 32:1757–1762.
Doern G.V (1995). Susceptibility tests of fastidious bacteria. Manual of Clinical Microbiology, 6th edition, Murray P.R, Baron E.J, Pfaller M.A, Tenover F.C, Yolken R, American Society for Microbiology, Washington DC, Pp. 1342-1349.
Funke G, Monnet D, deBernardis C, von Graevenitz A, Freney J (1998). Evaluation of the VITEK 2 system for rapid identification of medically relevant Gram-negative rods. J Clin Microbiol, 36:1948–1952.
Garcia L.S (2010). Clinical Microbiology Procedures Handbook. Third edition. American Society of Microbiology Press, USA.
Hart C.A (1998). Antibiotic Resistance: an increasing problem? BMJ, 316:1255-1256.
Livermore D.M, Winstanley T.B, Shannon K.P (2001). Interpretative reading: recognizing the unusual and inferring resistance mechanisms from resistance phenotypes. J Antimicrob Chemother, 48 Suppl 1:87-102.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of Microorganisms, 12th edition. Pearson Benjamin Cummings Inc, USA.
Mahon C. R, Lehman D.C and Manuselis G (2011). Textbook of Diagnostic Microbiology. Fourth edition. Saunders Publishers, USA.
National Committee for Clinical Laboratory Standards. Performance Standards for antimicrobial susceptibility testing. 8th Informational Supplement. M100 S12. National Committee for Clinical Laboratory Standards, 2002. Villanova, Pa.
Washington J.A (1993). Rapid antimicrobial susceptibility testing: technical and clinical considerations. Clin Microbiol Newsl, 15:153–155.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.