In recent times, antibiotic resistance of pathogens to drugs (antibiotics) directed towards the degrading properties of microbes in vivo has been on the increase both in the community and in the hospital. Antibiotics are exceptionally vital in clinical medicine for the treatment of bacterial related infections, but unfortunately bacteria are capable of developing resistance to them. Antibiotic resistance is a global health problem that has bedeviled our health sector worldwide, affecting both the developed and developing countries of the world. They make infectious diseases very difficult to treat. The emergence of antibiotic resistance is a complex problem that is driven by many interconnected factors, of which the use and misuse of antimicrobial agents (antibiotics, antiseptics, disinfectants, and preservatives) amongst other factors, is the main driving force for the development of resistance.
Antibiotic resistance occurs when bacteria change in some way that reduces or eliminates the effectiveness of drugs, chemicals or agents designed to cure or prevent the infection. Thus, the bacteria survive and continue to multiply causing harm and havoc in the patient (host) taking the drug. There has been a very great concern that the “antibiotic era” might be coming to an end – firstly, because the rate of production of new drugs has diminished greatly and, secondly, because microbes (viruses, bacteria, fungi, protozoa) are showing great inventiveness in devising mechanisms for circumventing the inhibiting and killing properties of drugs (antibiotics) directed towards them. Deaths from acute respiratory infections, diarrheal diseases, measles, AIDS, malaria and tuberculosis account for more than 85% of the mortality from infection worldwide. Resistance of microbes to first-line drugs causing these diseases according to the WHO ranges from zero to almost 100% and in some cases, resistance to both second – and third – line drugs is seriously compromising treatment outcome.
Antimicrobial resistance (AMR) is a public health menace occurring in both the hospital and general environments of both developed and developing countries, and it has the ability to launch a post-antibiotic era – where no antibiotics will be efficacious enough to handle infectious diseases of microbial origin if nothing is done to mitigate it early on. AMR occurs when bacteria change over time and no longer respond to antibiotics; thus infections become untreatable, leading to severe illness, long hospitalization, death and economic loss.
According to a recent report, 10 million deathsper year will be caused by AMR by 2050.3 AMR is one of the greatest threat to human health, animal health, food security and food safety. This is because antibiotics are used in both human and animal medicine; and in most cases, they are used at sub-inhibitory levels not lethal enough to kill-off the infecting bacteria. Consequently, the surviving bacteria strains go on to develop resistance mechanisms against the antimicrobial agents they were exposed to; and this gives them exceptional ability to ward-off their killing or inhibitory effects in the future. AMR bacteria and genes evolve continuously as a natural mechanism to ward-off the antimicrobial onslaughts of antimicrobial agents; however, they are easily selected following the application of antibiotics/antimicrobial agents especially irrationally and at sub-inhibitory concentrations in both hospital milieus and the general environment. This makes it easy for AMR bacteria and genes to evolve and spread between humans and animals and the environment. More worrisome is the fact that the rate at which bacteria evolves resistance to available antibiotics is not at par with the development of novel antimicrobial agents to counter this global crisis of AMR.
Self-medication is one major factor driving the spread of AMR in most part of the world, especially in places where there is less-controlled use of antibiotics in human or animal health. In Nigeria for example, majority of people who are being treated for malaria (caused by Plasmodium – a protozoan) will most often be given antibacterial agents targeting the pathogen that causes typhoid fever (Salmonella) in addition to the anti-malarial drug. Such phenomenon will result to the evolution of AMR due to selective pressure which allows bacteria to become resistant following undue exposure of the pathogen to antibiotics.
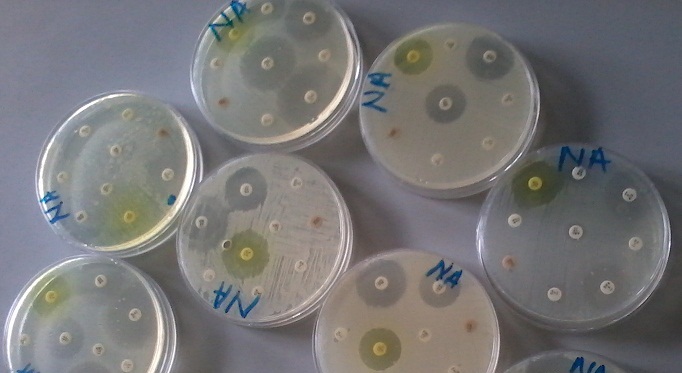
A major example is extended spectrum β – lactamase (ESBL) – producing bacteria which is resistant to virtually all beta – lactam drugs and some non – beta lactam drugs. Antibiotic resistance though a natural biological phenomenon, has in no doubt lead to the loss in the efficacy of some important drugs (especially the beta-lactams) from our therapeutic armamentarium. Nobody is to be blamed for this plethora of menace that is gradually eroding the efficacy of our drugs, since the introduction of every antimicrobial agent into clinical practice at one time or the other has been followed by the detection in the laboratory of strains of microorganisms that are resistant to these antimicrobial agents. In containing antibiotic resistance in both our community and the hospital, a good and adequate routine diagnostic antimicrobial susceptibility testing in the microbiology laboratory is paramount.
They should be charged with the responsibility of detecting antibiotic resistant strains of microbes (especially ESBL – producing bacteria) in the hospitals and in the community using internationally recognized protocol as outlined by the Clinical Laboratory Standard Institute, CLSI (formerly National Committee for Clinical Laboratory Standards) guideline. Data emanating from such studies should be made available and harnessed properly by all stakeholders in order to develop a road map for the proper control and eradication of antibiotic resistance from our world. Therefore, it is ripe for us to close the door on antibiotic resistant strains of bacteria before we wake up someday and find out that the only weapon (antibiotics) we have against bacterial related diseases have left us.
References
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Bisht R., Katiyar A., Singh R and Mittal P (2009). Antibiotic Resistance – A Global Issue of Concern. Asian Journal of Pharmaceutical and Clinical Research, 2 (2):34-39.
Courvalin P, Leclercq R and Rice L.B (2010). Antibiogram. ESKA Publishing, ASM Press, Canada.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA.
Fernandes Prabhavathi (2006). Antibacterial discovery – the failure of success? Nature Biotechnology, 24(12):1.
Finch R.G, Greenwood D, Norrby R and Whitley R (2002). Antibiotic and chemotherapy, 8th edition. Churchill Livingstone, London and Edinburg.
Hart C.A (1998). Antibiotic Resistance: an increasing problem? BMJ, 316:1255-1256.
Jayaramah R (2009). Antibiotic Resistance: an overview of mechanisms and a paradigm shift. Current Science, 96(11):1475-1484.
Mascaretti O.A (2003). Bacteria versus antibacterial agents: An integrated approach. Washington: ASM Press.
Mascaretti O.A (2003). Bacteria versus antimicrobial agents: An Integrated Approach. Washington: ASM Press.
Mazel D and Davies J (1998). Antibiotic Resistance: The Big Picture. In B. Rosen and S. Mobashery (Eds). Resolving the antibiotic paradox: progress in understanding drug resistance and developments of new antibiotics. New York: Plenum Press.
Russell A.D and Chopra I (1996). Understanding antibacterial action and resistance. 2nd edition. Ellis Horwood Publishers, New York, USA.
Sundsfjord A., Simonsen G.S., Haldorsen B.C., Haaheim H., Hjelmevoll S., Littauer P and Dahl K.H (2004). Genetic methods for detection of antimicrobial resistance. APMIS, 112:815-37.
Twyman R.M (1998). Advanced Molecular Biology: A Concise Reference. Bios Scientific Publishers. Oxford, UK.
Weaver R.F (2005). Molecular Biology. Third edition. McGraw-Hill Publishers, USA.
Willey J.M, Sherwood L.M and Woolverton C.J (2008). Harley and Klein’s Microbiology. 7th ed. McGraw-Hill Higher Education, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.