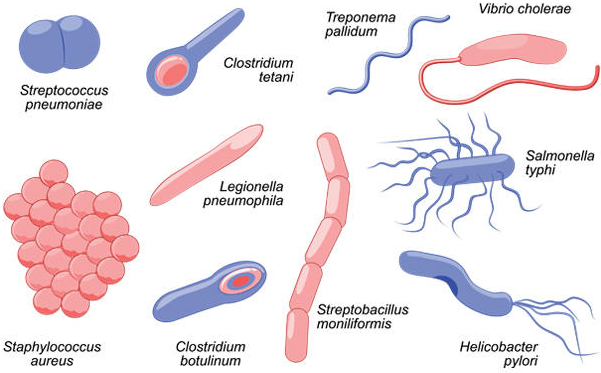
Neisseria gonorrhoeae is a Gram-negative, oxidase-positive, non-motile, non-sporulating, non-capsulate, diplococcus found asymptomatically in humans. N. gonorrhoeae is found in the family Neisseriaceae and genus Neisseria which contains two important human pathogens viz: N. gonorrhoeae and N. meningitidis (which causes meningococcal meningitis, an inflammation of the meninges of the brain and spinal cord). Though the syndromes of the diseases caused by N. gonorrhoeae and N. meningitidis sometimes have common characteristics; the former causes genital infections in the genitourinary tract while the latter causes meningitis in the upper respiratory tract of humans.
Other species of Neisseria are usually commensal organisms that occupy the alimentary and upper respiratory tract of humans; and these species are harmless. It causes gonorrhea, a sexually transmitted infection (STI) in humans (both male and female). N. gonorrhoeae, a bacterium known to occur in pairs (i.e. diplococcus)can also be called gonococcus. Gonorrhea is usually symptomatic in men and asymptomatic in women. The genitourinary tract, conjunctiva of the eye, pharynx, throat, and the rectum are usually the parts of the body that are affected in N. gonorrhoeae infection. In men, the urethra, epididymis, bladder and prostrate are usually affected by the organism but N. gonorrhoeae colonizes the urethra more than these other parts causing urethritis and dysuria (difficulty in urination).
But in women, N. gonorrhoeae infects the cervix, rectum, urethra and vulva. In women, infertility or ectopic pregnancy (i.e. development of the embryo in the fallopian tube instead of the uterus) can result following N. gonorrhoeae colonization of the pelvis (where it causes pelvic inflammatory disease, PID). Sexual intercourse especially with an infected individual is the primary route via which this pathogen can be acquired and transmitted. The endocervix and urethra are mostly affected in females, but in males the urethra is the most affected organ. However, N. gonorrhoeae is notorious for spreading to other vital organs and tissues of the body (especially the parts of the body with mucous membranes) where it causes similar infection.
Gonorrhea infection in women can also facilitate the easy contraction of HIV due to the inflammation of the genital region which allows the virus to gain entry during sexual intercourse. Ophthalmic neonatorum (blindness in neonates) can also occur in newborn infants whose mother’s vagina is infected with N. gonorrhoeae. The infant’s eye primarily become infected with gonococcus during delivery, and if left untreated the child can go blind. Occasionally, epididymitis (inflammation of the epididymis) can occur in men.
PATHOGENESIS OF NEISSERIA GONORRHOEAE INFECTION
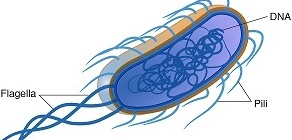
Upon invasion, N. gonorrhoeae attaches to the mucosal surfaces of the urethra in males and cervix in female using its pili, fimbriae and other adherence molecules (known as adhesins). This initial attachment sparks up a local inflammatory reaction at the site of invasion (which includes the rectum, throat and eye), and attachment and penetration of the microbe into the host cell is largely made possible by the action of the pili and adhesins. Symptoms of gonorrhea vary greatly in both males and females. In females, the disease is often unrecognized due to the similarity of infection to other vaginal infections caused by non-gonorrheal microbes.
The most common symptom of gonorrhea in adult male’s aside urethritis and dysuria may include frequent painful urination, and the discharge of scanty, clear or cloudy and purulent fluid. Purulent vaginal discharges are the major symptom of the disease in adult females who are usually covert with the infection. N. gonorrhoeae specifically attaches to the columnar epithelial cells of the urogenital tract with its surface protein, opacity associated protein (Opa) and other adhesins that allows it to do so. N. gonorrhoeae is sensitive to drying and can rarely survive outside the mucous membranes of the genitourinary tract of its human host.
Adhesion of gonococcus to the mucosal surfaces of the genitourinary tract prevents it from being washed away by the flushing action of the urine in males and the natural vaginal discharges in females. N. gonorrhoeae exhibit a complex and heterogeneous antigenic structure that is capable of mutation, and its outer membrane is composed of numerous surface pili and other phospholipid molecules including lipooligosaccharide (LOS), lipopolysaccharides (LPS), and adherence protein molecules called protein II or Opa proteins all of which enhances its pathogenicity and virulence in vivo. Infection with gonococcus is predominantly through a direct and intimate person-to-person sexual contact, and painful urination (in males) and unusual purulent vaginal discharge (in females) are the most important syndromes that follow infectivity.
After invasion and attachment, N. gonorrhoeae becomes engulfed by phagocytes as they invade epithelial cells, and once intracellular, the host immune system will have little or no effect on it. LOS, LPS and the Opa proteins (which are adhesins) helps to defend gonococcus against innate immune system attack in vivo.LOS and bacterial peptidoglycan are released by autolysis, and LOS is believed to stimulate the production of tumor necrosis factor (TNF) which causes cell damage. Gonococcus infection is usually limited to its site of entry where it cause local injury and inflammation, and can rarely spread to the blood stream or other vital tissues of the body.
Several disseminated bacterial infections including PID, gonorrheal bacteremia, gonorrheal arthritis, and gonorrheal endocarditis can ensue following the spread and dissemination of gonococcus in the body. These later infection are generally referred to as disseminated gonococcal infections (DGIs). Anal intercourse (especially in homosexual males) can also result to a variety of symptomatic rectal infections in persons engaging in such activity.
LABORATORY DIAGNOSIS OF NEISSERIA GONORRHOEAE INFECTION
Centrifugedurine, urethral exudates, and cervical exudates are the main specimens collected in suspected cases of N. gonorrhoeae infection. Rectal swab can also be obtained from patients suspected to have engaged in anal sex, and who may have presented clinical syndromes of rectal infections. Gram smear of genitourinary samples which demonstrates the kidney-bean shape of the microbe (i.e. Gram-negative diplococci within a neutrophil) is predominantly the most important laboratory diagnostic decisive factor for gonorrhea especially in adult males.
Gram smear is rarely used to diagnose the disease in infected females due to morphological similarity of other bacteria from the female vagina with gonococcus. Gram smears of urethral exudates on swab sticks should be rolled onto clean glass slide immediately after collection, fixed (using methanol) and stained without any prior immersion in normal saline. It is noteworthy that smear should always be made prior to culture of suspected specimens. Aside Gram smear, culture of genital samples (e.g. cervical exudates from females) on growth media is necessary to determine biochemical reaction, colony and cell morphology of the microbe.
Throat swabs can also be obtained from patients engaging in oral sex for culture. Gonococcus is a very sensitive organism, thus care must be taken in handling specimen, selecting culture media and in analyzing culture results in order to differentiate the pathogen from normal microflora of the body. N. gonorrhoeae produces small, raised, translucent or grey colonies after one or two days of culture or overnight incubation in the presence of CO2 at 35oC. N. gonorrhoeae is a fastidious, aerobic or facultative microbe, and thus requires additional nutrient (e.g. blood and animal protein) for growth in selective or enriched culture media such as the Modified New York City medium (Figure 1).It occurs intracellularly and extracellularly in its host cell, but it is typically seen as diplococcus in pus (polymorphonuclear) cells.
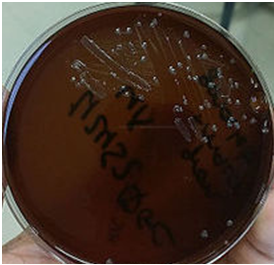
N. gonorrhoeae grows well on chocolate agar and on other enriched medium including Martin-Lewis medium and Thayer Martin medium (each of which contain antibiotics that inhibit bacteria and fungi) that enhances its growth. Serological investigations including the use of PCR for DNA amplification and DNA probe has also been developed for the laboratory diagnosis of gonococcus infection.
IMMUNITY TO NEISSERIA GONORRHOEAE INFECTION
Infection with gonococcus does not confer any form of protection against the pathogen, thus antibody response to organism is weak. N. gonorrhoeae infection is a re-occurring bacterial infection, thus immunity against re-infection is often not possible especially due to the antigenic variation of the microbe. Though antibodies (including IgA and IgG) are produced following N. gonorrhoeae infection in human hosts, their level is very insignificant in provoking any effective immune response.
The low level of antibody production in gonococcus infection coupled with the antigenic variation of N. gonorrhoeae (exemplified in Opa, LOS, pili) strains allows the microbe to evade hosts immune surveillance and remain undetected and unperturbed in vivo. Repeated infection with gonococcus is a common phenomenon in sexually active individuals especially in those with multiple partners (who may be harbouring the pathogen).
In addition, the antibodies produced during gonococcus infection are usually strain-specific (i.e. produced against a particular N. gonorrhoeae strain which may be genetically different from the invading microbe) and cannot provide cross-immunization in the disease.
TREATMENT OF NEISSERIA GONORRHOEAE INFECTION
In the past, gonorrhea was successfully treated with penicillin G (which is administered intramuscularly), but the development of resistance mechanisms including β-lactamase enzymes and alteration of N. gonorrhoeae penicillin-binding-proteins (PBPs) due to the widespread use of penicillin has made this antibiotic to be ineffective for treating gonorrhea.
Currently, the center for disease control and prevention (CDC) recommends the use of fluoroquinolones (e.g. levofloxacin, ofloxacin and ciprofloxacin) and third-generation cephalosporins (e.g. cefixime, ceftriaxone) which can either be administered orally or intramuscularly for the treatment of gonorrhea.
Antibiotics such as azithromycin, erythromycin, or doxycycline are also included in the treatment options for gonococcus infected patients due to the possibility of co-infection with other STIs including syphilis and Chlamydia trachomatis infection.
Gonorrhea infection is incomplete if sex partners are left out. Due to the asymptomatic nature of the infection in females, it is critical to refer and treat sex partners of infected individuals in order to avoid the recurrence of the disease in the treated patient.
PREVENTION AND CONTROL OF NEISSERIA GONORRHOEAE INFECTION
According to WHO, gonorrhea and other related sexually transmitted infections (STIs) has developed resistance to many of the commonly available antibiotics used for the treatment of the disease, and this portend grave danger to those with the disease and even in the management of newer infections. In addition, over 500 million STIs (including gonorrhea) are estimated to occur worldwide every year triggering a range of sexual, reproductive, and maternal-child health problems. N. gonorrhoeae infection occurs worldwide, and the disease is transmitted exclusively by sexual contact through adult men and women that are covert of the infection.
Gonorrhea is a common and costly preventable STI that is of public health concern. Awareness and education of the general public, coupled with proper treatment of infected patients especially those that are covert are very paramount to the control and prevention of N. gonorrhoeae infection. Avoiding multiple sexual partners and remaining faithful to one’s partner are critical in preventing the spread and transmission of the disease. Use of protection (e.g. condoms) during sexual intercourse can also confer some level of protection. High-risk population should be discovered, screened and properly treated to break the mechanical chain of transmitting the infection.
Ophthalmic neonatorum can be prevented in newborns by topical application of tetracycline or erythromycin creams. Infected females show little or nor signs of N. gonorrhoeae infection, and thus, such individual with multiple sex partner can easily infect many males as possible. Though social stigmas associated with gonorrhea and other STIs may make it difficult to identify such individuals for proper treatment in order to break the chain of transmission; gonorrhea can be controlled if such individuals and sexual contacts of infected people are identified and treated immediately.
Lactic acid bacteria which is a normal flora found in the vagina of adult females maintains a pH that makes it difficult for pathogenic bacteria including gonococcus to thrive. But the continued use of oral contraceptives by women (an agent that induces the body to mimic pregnancy) modifies the mucosal surfaces of the female genitalia, and this favours the development of N. gonorrhoeae which go on to colonize mucosal milieu of the vagina where vaginal pH has been increased and glycogen production reduced following the action of oral contraceptives. Such conditions make it difficult for lactic acid bacteria to develop, and this facilitates the genitourinary tract colonization by gonococcus which is transmitted from an infected male partner.
Infectivity with gonococcus is often greater in females than in males even though adult females are usually asymptomatic. The antigenic switches of N. gonorrhoeae (which has made gonococcus to continually dodge the host’s immune system attack) have made it difficult to develop effective vaccine against the pathogen. An understanding of the antigenic variation and mechanisms with which gonococcus uses to evade the immune response of its host is very critical to the development of an effective vaccine against this dreaded human pathogen.
OTHER SPECIES OF NEISSERIA
- Neisseria meningitidis: – Neisseria meningitidis causes meningitis and other forms of meningococcal disease such as meningococcemia, a life-threatening sepsis in humans.
- Neisseria mucosa: N. mucosa is notable because of its ability to metabolize the sugar, sucrose; and it is also implicated as a causative agent in endocarditis. N. mucosa is part of the normal human nasopharyngeal flora and infrequently causes human infections, including meningitis.
- Neisseria sicca: Neisseria sicca is considered to be part of the normal flora of the oropharynx; and though usually believed to be a harmless saprophyte, it has rarely been recognized as an etiologic agent in human disease, particularly in immunodeficient hosts – where it causes pneumonia.
- Neisseria cinerea: Neisseria cinerea is a non-pathogenic bacterium that has been isolated from numerous infections including acute meningitis; and the organism is known to colonize the oropharynx and the genital tract.
- Neisseria subflava: Neisseria subflava is a common inhabitant found in the human upper respiratory tract as a normal flora. It is considered non-pathogenic but the organism can cause postoperative meningitis in rare cases.
- Neisseria lactamica: Neisseria lactamica is a part of the normal flora of the upper respiratory tract of humans especially infants and young children; and it shares this ecological niche with Neisseria meningitidis (the causative agent of meningitis).
- Neisseria flavescens:N. flavescens play a pathogenic role in immunocompromised and diabetic individuals; and it has been linked to meningitis, pneumonia, empyema, endocarditis, and septicemia in rare cases. The organism is commonly isolated from the cerebrospinal fluid of infected individuals.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.