Bacteria have evolved to survive in diverse environments. They survive exposure to harsh chemicals including antibiotics, and they also survive difficult growth conditions. They have learned to “detoxify” harmful substances e.g. antibiotics.
Antibiotic resistance can either be intrinsic or acquired.
INTRINSIC (INNATE) RESISTANCE
Some bacteria are said to possess innate/intrinsic resistance against antibacterial action put forward by antibiotics. Others are even naturally resistant to the antimicrobial agent that they synthesize. For example, Streptomyces are antibiotic synthesizing bacteria normally isolated from the soil; and they have immunity to the antibiotic that they synthesize. Microorganisms that are inherently resistant mount a great ingenuity in devising means or ways of neutralizing the killing or inhibiting action of antibiotics directed towards them.
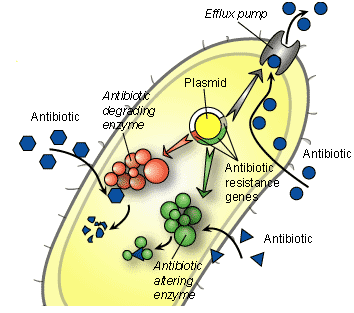
This innate form of antibiotic resistance in bacteria shows the different variations in the structure of the cell envelope of the organism, which allows them to mount resistance against drugs. The outer cell membrane of Gram negative bacteria, lack of antibiotic target site on bacteria and the influx-efflux mechanisms of some pathogenic bacteria are some natural ways by which microbes build up resistance against antimicrobial onslaught (Figure 1).
It is a vertical means by which bacteria acquire resistance. Intrinsic or innate form of antibiotic resistance can occur by any one of the following route:
- Spontaneous mutation in the chromosomal DNA of bacteria.
- Accumulation of several point mutations in bacteria.
- An evolutionary process occurring only under selective pressure e.g. prior exposure of bacteria to antibiotics.
ACQUIRED (PHENOTYPIC) RESISTANCE
This type of antibiotic resistance is acquired by bacteria from the environment or other microorganisms by one of the means of genetic transfer (conjugation, transformation, and transduction). In acquired/phenotypic resistance, the bacteria acquire reduced susceptibility to antibiotics through adaptation to growth within a specific environment.
Pathogenic bacteria can develop resistance to a particular drug after prior unwarranted exposure to antimicrobial agents. In such scenarios, the microbes are taught to remain active even in the face of potent antimicrobial onslaught. Acquired resistance is a horizontal means by which bacteria become resistant to antibacterial properties of antibiotics. This form of antibiotic resistance can be achieved in bacteria by one of the following route:
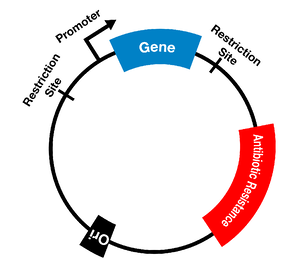
- Resistance can be maintained on horizontal mobile elements like plasmids, integrons and transposons which can be transferred to susceptible organisms.
- Resistant genes can be transferred among bacteria through means of genetic transfer.
- Resistance genes can be integrated into the bacterial chromosome or can be maintained in an extra chromosomal state (e.g. plasmids).
- Changes in the genome of an organism (i.e. mutation) can predispose an organism to becoming resistant to antimicrobial agents.
References
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Bisht R., Katiyar A., Singh R and Mittal P (2009). Antibiotic Resistance – A Global Issue of Concern. Asian Journal of Pharmaceutical and Clinical Research, 2 (2):34-39.
Courvalin P, Leclercq R and Rice L.B (2010). Antibiogram. ESKA Publishing, ASM Press, Canada.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA.
Fernandes Prabhavathi (2006). Antibacterial discovery – the failure of success? Nature Biotechnology, 24(12):1.
Finch R.G, Greenwood D, Norrby R and Whitley R (2002). Antibiotic and chemotherapy, 8th edition. Churchill Livingstone, London and Edinburg.
Hart C.A (1998). Antibiotic Resistance: an increasing problem? BMJ, 316:1255-1256.
Jayaramah R (2009). Antibiotic Resistance: an overview of mechanisms and a paradigm shift. Current Science, 96(11):1475-1484.
Mascaretti O.A (2003). Bacteria versus antibacterial agents: An integrated approach. Washington: ASM Press.
Mascaretti O.A (2003). Bacteria versus antimicrobial agents: An Integrated Approach. Washington: ASM Press.
Mazel D and Davies J (1998). Antibiotic Resistance: The Big Picture. In B. Rosen and S. Mobashery (Eds). Resolving the antibiotic paradox: progress in understanding drug resistance and developments of new antibiotics. New York: Plenum Press.
Russell A.D and Chopra I (1996). Understanding antibacterial action and resistance. 2nd edition. Ellis Horwood Publishers, New York, USA.
Sundsfjord A., Simonsen G.S., Haldorsen B.C., Haaheim H., Hjelmevoll S., Littauer P and Dahl K.H (2004). Genetic methods for detection of antimicrobial resistance. APMIS, 112:815-37.
Twyman R.M (1998). Advanced Molecular Biology: A Concise Reference. Bios Scientific Publishers. Oxford, UK.
Weaver R.F (2005). Molecular Biology. Third edition. McGraw-Hill Publishers, USA.
Willey J.M, Sherwood L.M and Woolverton C.J (2008). Harley and Klein’s Microbiology. 7th ed. McGraw-Hill Higher Education, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.