Antibiotic resistance is a phenomenon that occurs when bacteria are not killed or inhibited by usually achievable systemic concentration of an antibiotic (drug) with normal dosage schedule and/or fall in the minimum inhibitory concentration ranges of the drug in question. It occurs when bacteria change in some way that reduces or eliminates the effectiveness of drugs or other agents designed to cure or prevent the infection.
Thus the bacteria survive and continue to multiply causing more harm in the host taking the drug. Pathogenic bacterial strains that are resistant to some available conventional antibiotics are constantly emerging in both the community and hospital settings. And this has been greatly attributed to the misuse of these agents both for human and non-human purposes. Antibiotic resistance is a natural phenomenon and it is exacerbated following the prior administration of an antibiotic.
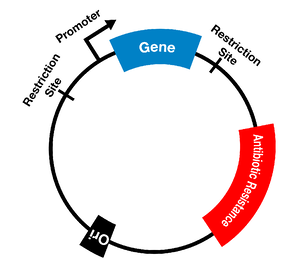
According to the World Health Organization (WHO), the introduction of every antimicrobial agent into clinical practice has been followed by the detection in the laboratory of strains of microorganisms that are resistant, i.e. able to multiply in the presence of drug concentrations higher than the concentrations in humans receiving therapeutic doses. Microorganisms harbor resistance genes which encode various mechanisms that allow them to resist the killing or inhibitory effects of specific antibiotics directed towards them. These mechanisms also offer resistance to other antibiotics or antimicrobial agents of the same class and sometimes to several different antimicrobial classes.
Microbial infections involving resistant strains of microbes result in treatment failure and antibiotic options are limited because it takes time to decipher the resistant profile of the infecting organism, and because the organisms is able to thrive even in the face of agents capable of inhibiting its growth and survival, the possibility of causing infection in a susceptible human host through transmission is feasible.
The problem of antibiotic resistance is a vital topic and a global health problem that has received increasing attention over the last two decades. It is certainly not a new topic neither was it unpredictable. When antibiotic resistance occurs, it is the microbe (bacterium) that is resistant, not the antibiotic nor the patient or host taking it. Species of bacteria that are normally resistant to penicillin for example, can develop resistance to these drugs either through mutation (vertical transmission) or through acquisition from other bacteria of resistance genes (horizontal transmission).
This dual means of acquiring resistance explains why the resistance trait can spread rapidly and replace a previously drug – susceptible population of bacteria. Antibiotic resistance is on the rise threatening our ability to treat infectious diseases and even some of those that cause most deaths in the past (e.g. tuberculosis).
Diseases such as tuberculosis, which once thought to be under control, are now becoming increasingly difficult to treat. This is because available medicines become less effective following the emergence of resistance forms of microbes that steadily depletes the arsenal of drugs available for therapy.
References
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Bisht R., Katiyar A., Singh R and Mittal P (2009). Antibiotic Resistance – A Global Issue of Concern. Asian Journal of Pharmaceutical and Clinical Research, 2 (2):34-39.
Courvalin P, Leclercq R and Rice L.B (2010). Antibiogram. ESKA Publishing, ASM Press, Canada.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA.
Ejikeugwu Chika, Iroha Ifeanyichukwu, Adikwu Michael and Esimone Charles (2013). Susceptibility and Detection of Extended Spectrum β-Lactamase Enzymes from Otitis Media Pathogens. American Journal of Infectious Diseases. 9(1):24-29.
Ejikeugwu Chika, Ugwu C.M., Ikegbunam N.M, Araka C.O., Iroha I.R., Adikwu M.U and Esimone C.O (2012). Evaluation of antibacterial activity of the leave extracts of Buchholzia coriacea. Asian Journal of Pharmaceutical and Biological Research. 2(4):204-208.
Ejikeugwu Chika, Ugwu Malachy, Iroha Ifeanyichukwu, Gugu Thaddeus, Duru Carissa, Eze Peter, and Esimone Charles (2013). Detection and antimicrobial susceptibility of some Gram negative bacteria producing carbapenemases and extended spectrum beta lactamases. International Journal of Microbiology and Immunology Research, 2(6):064-069.
Ejikeugwu Chika, Umeokoli Blessing, Iroha Ifeanyichukwu, Ugwu Malachy, Esimone Charles (2015). Phytochemical and Antibacterial Screening of Crude Extracts from Leaves of Wonderful Kola. American Journal of Life Sciences. Special Issue: Microbiology Research, 3(2):5-8.
Ejikeugwu P.C., Ugwu C.M., Araka C.O., Gugu T.H., Iroha I.R., Adikwu M.U and Esimone C.O (2012). Imipenem and Meropenem resistance amongst ESBL producing Escherichia coli and Klebsiella pneumoniae clinical isolates. International Research Journal of Microbiology. 3(10):339-344.
Fernandes Prabhavathi (2006). Antibacterial discovery – the failure of success? Nature Biotechnology, 24(12):1.
Mazel D and Davies J (1998). Antibiotic Resistance: The Big Picture. In B. Rosen and S. Mobashery (Eds). Resolving the antibiotic paradox: progress in understanding drug resistance and developments of new antibiotics. New York: Plenum Press.
Russell A.D and Chopra I (1996). Understanding antibacterial action and resistance. 2nd edition. Ellis Horwood Publishers, New York, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.