Enterococcus (plural: Enterococci) is a group of bacteria that is normally found in the intestines of humans and many animals. Two species of Enterococci, which are found in the body of healthy individuals, are Enterococcus faecalis and Enterococcus faecium.
Both E. faecalis and E. faecium are associated with human diseases; and they are mostly involved as causative agents in some gastrointestinal infections of humans. E. faecalis and E. faecium can sometimes cause infections of the urinary tract system, wounds or bloodstream infections, particularly in immunocompromised individuals.
Vancomycin is a type of antibiotic that is often used to treat enterococcal infections in humans. However, many strains of Enterococci have become resistant to this antibiotic (i.e., vancomycin) and other glycopeptides such as teicoplanin. This group of vancomycin-resistant enterococci is known as VRE.
Six types of acquired vancomycin resistance in enterococci are now known but only two of them are widely prevalent. These acquired vancomycin resistance genes are vanA and vanB. Both vanA and vanB are mostly associated with E. faecium infection.
Infections with VRE predominantly occur in hospital environments; and thus, VRE are mostly implicated in nosocomial infections i.e., hospital acquired infections. Serious VRE infections often result in prolonged treatment and hospitalization. The reason for the long hospital stays due to VRE infection is because the therapeutic options in the face of VRE are often limited.
The limitation of therapeutic options for the treatment of infections caused by antibiotic resistant bacteria is not only in the case of VRE, but this is also applicable to other resistant organisms including ESBL- and MBL-producing bacteria. Such a scenario often poses challenge to the physician who is often in a quagmire when it comes to choosing antibiotic for the treatment of infections caused by resistant bacteria.
The major concern with VRE infections is that resistance to vancomycin could spread to other clinically significant species, such as Staphylococcus aureus. Today, there are strains of S. aureus known as methicillin resistant S. aureus – that is posing similar challenges of VRE in the hospital environment.
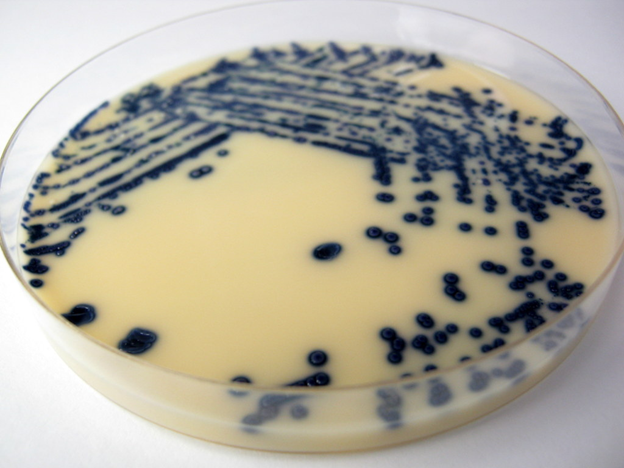
Detection of VRE in the laboratory: The best culture media for the detection of VRE in the hospital laboratory is Brilliance VRE agar (Figure 1). Brilliance VRE agar is a chromogenic screening plate for the detection of VRE, direct from clinical samples. And the detection of VRE using Brilliance VRE agar is just within 24 hours. Brilliance VRE agar also enables quick and easy screening of faecal samples, swabs and isolates of culture suspensions for VRE.
References
Werner G, Coque T.M, Hammerum A. M et al. (2008). Emergence and spread of vancomycin resistance among enterococci in Europe. Eurosurveillance, 13(47).
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.


