Subcutaneous mycoses are fungal infections that affect the subcutaneous tissues below the skin, and the bone and other tissues occasionally. The subcutaneous tissue or layer is the part of the skin that lies beneath the skin and it contain large deposits of fats (e.g. in the buttocks and thigh regions). Apart from affecting the subcutaneous tissues of the skin, subcutaneous mycoses also involve the dermis layer of the skin.
Dermis is the thick inner layer of the skin that lies beneath the epidermis, and it is the main layer of living skin cells. Subcutaneous mycoses rarely involve deeper tissues of the body even though they extend beneath the tissues that underlie the skin. This type of mycoses occurs when certain pathogenic fungi that reside in the soil and on plantation are introduced into the body via trauma or skin injury.
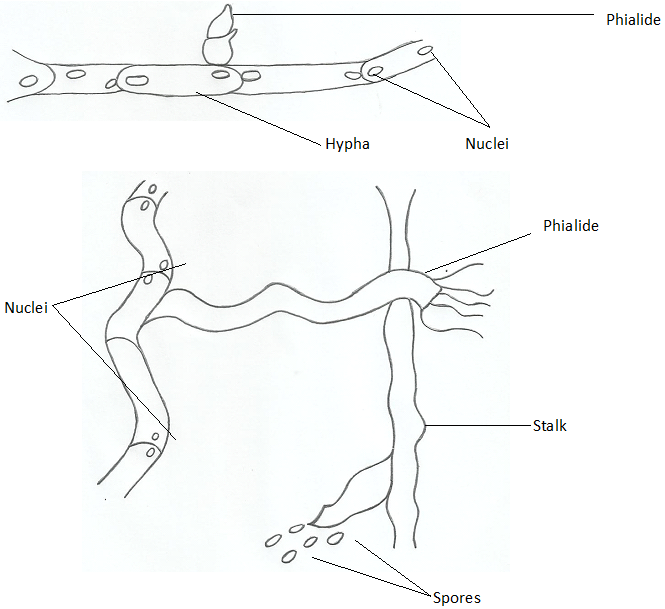
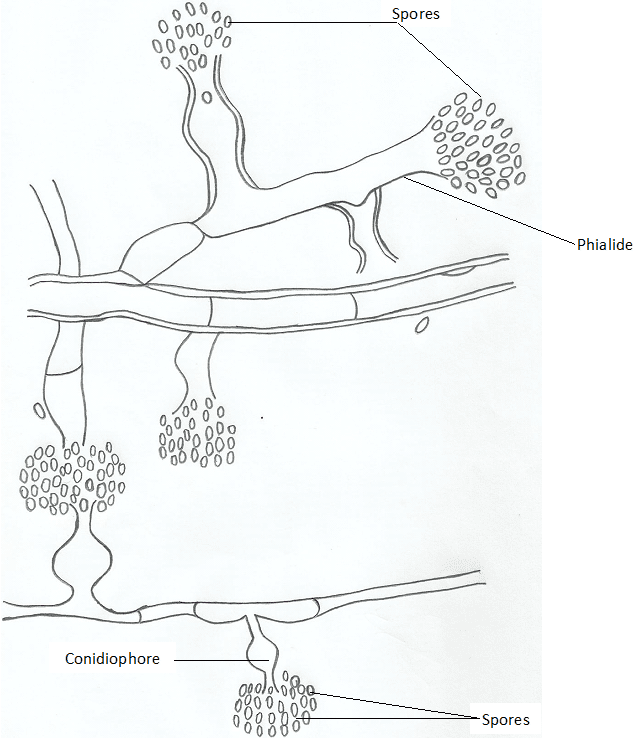
Subcutaneous mycoses include chromoblastomycosis (chromomycosis), sporotrichosis, mycetoma/madura foot (maduromycosis) and phaeohyphomycosis (Table 1). Chromoblastomycosisis caused by five recognized dematiaceous moulds which are Fonsecaea pedrosoi, F. compacta, Cladophialophora carrionii, Rhinocladiella aquaspersa and Phialophora verrucosa which form phialides.
Table 1. Synopsis of subcutaneous mycoses
| Mycoses | Causative agent | Clinical feature | Site of infection |
| Sporotrichosis | Sporothrix schenckii | Sporotrichosis is initiated following the traumatic introduction of S. schenckii conidia into the skin. It is usually characterized by granulomatous lesions at subcutaneous tissues of the skin. Lesions later become ulcerative or necrotic; and disease dissemination is rare but common in people with weakened immunity or debilitating disease such as cancer. | Subcutaneous tissues and lymphatic vessels |
| Chromomycosis (chromoblastomycosis) | P. verrucosa, C. carrionii, R. aquaspersa, F. pedrosoi, F. compacta | Chromomycosis is initiated following the traumatic introduction of any of the five dematiaceous moulds into the legs or foot. It is characterized by the formation of cauliflower-like and granulomatous nodules or lesions with black sclerotic or ulcerative bodies; and disease dissemination is rare. | Subcutaneous tissues of the legs and feet |
| Mycetoma (maduromycosis) or madura foot | Madurella mycetomatis, Exophiala jeanselmei, Acremonium falciforme, Pseudallescheria boydii, M. grisea amongst others | Mycetoma or madura foot is initiated following the traumatic inoculation of some specific fungal species in the soil into the foot. It is usually characterized by the development of oedematous and granulomatous nodules at the affected body site. Dissemination to bones and muscles may occur; and deformation & loss of function of affected tissues may also ensue. | Subcutaneous tissues of the feet, hands, thigh and head |
| Phaeohyphomycosis | Bipolaris species, Exophiala species, Wangiella species, Phialophora species amongst others | Phaeohyphomycosis is caused by the traumatic inoculation of dematiaceous moulds into the subcutaneous and cutaneous tissues. It is characterized by the formation of dark pigmented nodules in subcutaneous tissues. Sinusitis and brain abscess may occur but rare. | Subcutaneous tissues |
Microscopic illustrations of the mature and young phialides of P. verrucosa are shown in Figure 1 and Figure 2. The fungal agents that cause subcutaneous mycoses is numerous excluding sporotrichosis which is only caused by a particular fungus Sporothrix schenckii, a dimorphic fungus that is found in the soil and on agricultural plantations.
Sporotrichosis occur worldwide especially in tropical and subtropical countries; and the disease is initiated following an outdoor activity in which the fungus (S. schenckii)is inoculated into the host’s body via contaminated soil or materials. Granulomatous lesions are usually developed in the subcutaneous tissues that underlie the skin of S. schenckii infected individuals, and this may develop into an ulcerative lesion that is capable of dissemination via lymphatic vessels or bloodstream to other parts of the body.
Deep mycoses involving S. schenckii is rare; and lymphatic drainage of the infection when it occurs usually results in the development of multiple lesions in the affected individual. Sporotrichosis, an occupational disease common amongst gardeners, farmers and horticulturists is usually a self-limiting subcutaneous mycoses but treatment for the mycoses is usually done using oral antifungal agents (e.g. itraconazole or ketoconazole), oral administration of saturated potassium iodide solution and by surgical removal of lesions or nodules.
Most subcutaneous mycoses are occupational fungal diseases that mainly affect people who do or work in certain types of occupation such as miners, farmers, gardeners, horticulturists, forest keepers and florists. This is because the group of fungi that causes subcutaneous mycoses (as shown in Table 1) is ubiquitously found in the soil and on plants as saprophytic organisms. They only infiltrate the human body by chance via wound infections on the skin or through abrasions.
Pathogenic fungi that cause subcutaneous mycoses enter the body through traumatic inoculation or wound injury involving sharp contaminated objects or materials containing the infecting fungal organisms. After inoculation, the fungi or fungus migrate to the subcutaneous connective tissues and lymphatic vessels of the body (especially those that underlies the skin) where they elicit local, self-limiting and chronic fungal infections that usually results in the formation of granulomatous lesions.
Life-threatening infections associated with subcutaneous mycoses are rare in humans. But when deep or systemic mycoses due to subcutaneous fungal infection occur, the infections become broad and then affect other vital tissues and organs of the body such as the bones.
References
Anaissie E.J, McGinnis M.R, Pfaller M.A (2009). Clinical Mycology. 2nd ed. Philadelphia, PA: Churchill Livingstone Elsevier. London.
Beck R.W (2000). A chronology of microbiology in historical context. Washington, D.C.: ASM Press.
Black, J.G. (2008). Microbiology: Principles and Explorations (7th ed.). Hoboken, NJ: J. Wiley & Sons.
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA.
Brown G.D and Netea M.G (2007). Immunology of Fungal Infections. Springer Publishers, Netherlands.
Calderone R.A and Cihlar R.L (eds). Fungal Pathogenesis: Principles and Clinical Applications. New York: Marcel Dekker; 2002.
Chakrabarti A and Slavin M.A (2011). Endemic fungal infection in the Asia-Pacific region. Med Mycol, 9:337-344.
Champoux J.J, Neidhardt F.C, Drew W.L and Plorde J.J (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases. 4th edition. McGraw Hill Companies Inc, USA.
Chemotherapy of microbial diseases. In: Chabner B.A, Brunton L.L, Knollman B.C, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, McGraw-Hill; 2011.
Chung K.T, Stevens Jr., S.E and Ferris D.H (1995). A chronology of events and pioneers of microbiology. SIM News, 45(1):3–13.
Germain G. St. and Summerbell R (2010). Identifying Fungi. Second edition. Star Pub Co.
Ghannoum MA, Rice LB (1999). Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev, 12:501–517.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Larone D.H (2011). Medically Important Fungi: A Guide to Identification. Fifth edition. American Society of Microbiology Press, USA.
Levinson W (2010). Review of Medical Microbiology and Immunology. Twelfth edition. The McGraw-Hill Companies, USA.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of Microorganisms, 12th edition. Pearson Benjamin Cummings Inc, USA.
Mahon C. R, Lehman D.C and Manuselis G (2011). Textbook of Diagnostic Microbiology. Fourth edition. Saunders Publishers, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.