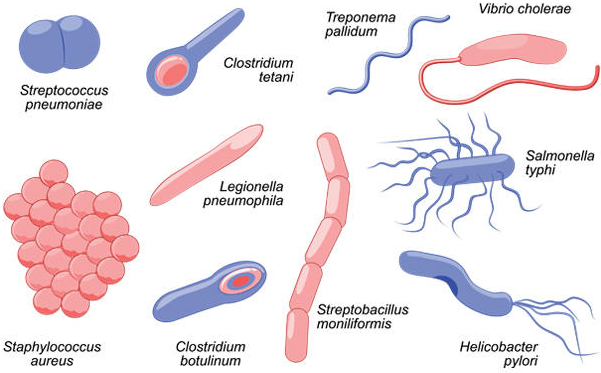
To establish an infectious disease, a disease agent (including bacteria, fungi, viruses and protozoa) must first come in contact with a susceptible human host. This phase is called contact or encounter. Humans first encounter with microorganisms starts immediately after birth (period in which the newborn begin to build up its own normal flora) but as the infant grows, he or she can come in contact with varying microorganisms (both harmless and pathogenic organisms) in the environment that are likely to cause an infection.
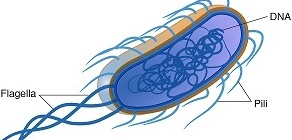
Adults can encounter pathogens from different routes including the air, food, water, fomites or via sexual intercourse. After a successful host-microbe encounter, pathogens begin to find their way into the host’s body via natural openings on the body (e.g. mouth, nose, ears, and vagina) or through wounds, cuts or abrasion on the skin. This phase is called invasion (Figure 1).
Microbes can also penetrate deeper tissues of the body via insect bites or through infected sharp objects. Upon entry into the body, the infectious agents begin to find their way to other organs and tissues far away from their point of entry. This phase is called spreading.
Microbes after spreading to their specific and target organs or tissues in the host, must be able to undergo reproduction in order to increase the number of infectious particle to a level that is necessary to establish an infection. This stage is called multiplication. Clinical signs and symptoms of a particular infectious process will not be noticeable until the microbial load in the host has reached the height that is considered necessaryto establish a disease condition.
It is worthy of note that there can still be some variations in some disease processes wheresignsand symptoms only appears after a given period of time (i.e. when the infectious agent is still at its window period). Also, some infectious agents produce toxins upon entering their hosts, and in such instances may not necessarily need to undergo multiplication before a disease or infection is established.
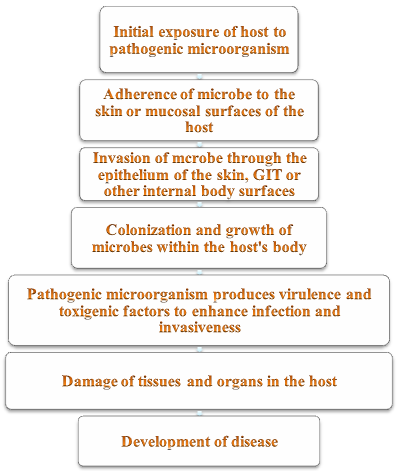
Infectious agents multiply successfully in the host through a variety of mechanisms including disruption of the host’s immune system, production of toxins and environmental conditions of the body.
Damage of the host’s organ(s) is the next step that follows multiplication of a microbe in vivo. Pathogens have the potential to damage and stop the normal function of one or more organs or tissues of their host, and this leads to a full blown disease. Some disease when not properly treated either therapeutically or via surgery can be wasting i.e. it can be a dead end in which the host eventually dies. If the host survives the pathogen invasion, both host and pathogen can coexist and continue to live together, and the asymptomatic individual can be a reservoir or source via which the microbe can infect a new susceptible host.
Host immune response (especially violent responses) to the body’s invasion by a microbe can sometimes lead to catastrophe in which some organs or tissues become affected. This can be seen in autoimmunity, in which the host’s immune response is directed against self or innate antigens of the body. Pathogenic microorganisms that cause diseases in humans may be endogenous (i.e. they are part of the normal flora of the body) or exogenous (i.e. they are microbes that penetrate the body from the outside).
Endogenous microorganisms can initiate an infection when the body’s immune system is compromised or when resident microflora becomes transient i.e. moved from its local position to a new location in the body while exogenous microorganisms are often acquired from the external environment such as from food, water, air or from inanimate objects and even from infected individuals.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.