The yellow fever virus is found in tropical and subtropical areas of Africa and South America. The virus is spread to people by the bite of an infected mosquito. Yellow fever is a very rare cause of illness in U.S. travelers. Illness ranges from a fever with aches and pains to severe liver disease with bleeding and yellowing skin (jaundice). Yellow fever infection is diagnosed based on laboratory testing, a person’s symptoms, and travel history. There is no medicine to treat or cure infection. To prevent getting sick from yellow fever, use insect repellent, wear long-sleeved shirts and long pants, and get vaccinated.
Prevention of Yellow Fever
The most effective way to prevent infection from Yellow Fever virus is to prevent mosquito bites. Mosquitoes bite during the day and night. Use insect repellent, wear long-sleeved shirts and pants, treat clothing and gear, and get vaccinated before traveling, if vaccination is recommended for you.
· Prevent Mosquito Bites
· Use Insect Repellent
Use Environmental Protection Agency (EPA)-registered insect repellents with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women.
- DEET
- Picaridin (known as KBR 3023 and icaridin outside the US)
- IR3535
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
- 2-undecanone
Tips for babies and children
- Always follow instructions when applying insect repellent to children.
- Do not use insect repellent on babies younger than 2 months old.
- Instead, dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
Tips for Everyone
- Always follow the product label instructions.
- Reapply insect repellent as directed.
- Do not spray repellent on the skin under clothing.
- If you are also using sunscreen, apply sunscreen first and insect repellent second.
Natural insect repellents (repellents not registered with EPA)
- We do not know the effectiveness of non-EPA registered insect repellents, including some natural repellents.
- To protect yourself against diseases spread by mosquitoes, CDC and EPA recommend using an EPA-registered insect repellent.
- Choosing an EPA-registered repellent ensures the EPA has evaluated the product for effectiveness.
Wear long-sleeved shirts and long pants
Treat clothing and gear
- Use permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels mosquitoes.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
Take steps to control mosquitoes indoors and outdoors
- Use screens on windows and doors. Repair holes in screens to keep mosquitoes outdoors.
- Use air conditioning, if available.
- Stop mosquitoes from laying eggs in or near water.
- Once a week, empty and scrub, turn over, cover, or throw out items that hold water, such as tires, buckets, planters, toys, pools, birdbaths, flowerpots, or trash containers.
- Check indoors and outdoors.
Prevent mosquito bites when traveling overseas
- Choose a hotel or lodging with air conditioning or screens on windows and doors.
- Sleep under a mosquito bed net if you are outside or in a room that does not have screens.
- Buy a bed net at your local outdoor store or online before traveling overseas.
- Choose a WHOPES-approved bed net: compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- Permethrin-treated bed nets provide more protection than untreated nets.
- Do not wash bed nets or expose them to sunlight. This will break down the insecticide more quickly.
Yellow Fever Vaccine
A safe and effective yellow fever vaccine has been available for more than 80 years.
- A single dose provides lifelong protection for most people.
- The vaccine is a live, weakened form of the virus given as a single shot.
- Vaccine is recommended for people aged 9 months or older and who are traveling to or living in areas at risk for yellow fever virus in Africa and South America.
- Yellow fever vaccine may be required for entry into certain countries.
Yellow Fever Vaccine Recommendations
Yellow fever vaccine is recommended for people who are 9 months old or older and who are traveling to or living in areas at risk for yellow fever virus in Africa and South America.
For most people, a single dose of yellow fever vaccine provides long-lasting protection and a booster dose of the vaccine is not needed. However, travelers going to areas with ongoing outbreaks may consider getting a booster dose of yellow fever vaccine if it has been 10 years or more since they were last vaccinated. Certain countries might also require a booster dose of the vaccine; visit Travelers’ Health for information on specific country requirements.
Talk to your healthcare provider to determine if you need a yellow fever vaccination or a booster shot before your trip to an area at risk for yellow fever.
Some people may have an increased risk of developing a reaction to the vaccine, but may still benefit from being vaccinated. These people, or their guardians, should talk to a healthcare provider about getting vaccinated:
- Between 6 and 8 months old
- Over 60 years old
- Pregnant
- Breastfeeding
A few people should not get the vaccine. Vaccine is not recommended for people who are:
- Allergic to a vaccine or something in the vaccine (like eggs)
- Aged 6 months or younger
- Organ transplant recipients
- Diagnosed with a malignant tumor
- Diagnosed with thymus disorder associated with abnormal immune function
- Diagnosed with a primary immunodeficiency
- Using immunosuppressive and immunomodulatory therapies
- Showing symptoms of HIV infection or CD4+ T-lymphocytes less than 200/mm3 (less than 15% of total lymphocytes in children aged 6 years or younger)
Reactions to Yellow Fever Vaccine
Reactions to yellow fever vaccine are generally mild and include headaches, muscle aches, and low-grade fevers. Rarely, people develop severe, sometimes life-threatening reactions to the yellow fever vaccine, including:
- Allergic reaction, including difficulty breathing or swallowing (anaphylaxis)
- Swelling of the brain, spinal cord, or the surrounding tissues (encephalitis or meningitis)
- Guillain-Barré syndrome, an uncommon sickness of the nervous system in which a person’s own immune system damages the nerve cells, causing muscle weakness, and sometimes, paralysis.
- Internal organ dysfunction or failure
If you recently received the yellow fever vaccination and develop fever, headache, tiredness, body aches, vomiting, or diarrhea, see your healthcare provider.
Some people may have an increased risk of developing a reaction to the vaccine, but may still benefit from being vaccinated. These people, or their guardians, should talk to a healthcare provider about getting vaccinated:
- Between 6 and 8 months old
- Over 60 years old
- Pregnant
- Breastfeeding
Yellow Fever Vaccine, Pregnancy, & Conception
Yellow fever vaccine has been given to many pregnant women without any apparent adverse effects on the fetus. However, since yellow fever vaccine is a live virus vaccine, it poses a theoretical risk.
Pregnant women should avoid or postpone travel to an area where there is risk of yellow fever. If travel cannot be avoided, discuss vaccination with your doctor.
While a two week delay between yellow fever vaccination and conception is probably adequate, a one month delay has been advocated as a more conservative approach.
If, for some reason, a woman is vaccinated during pregnancy, she is unlikely to have any problems from the vaccine and her baby is very likely to be born healthy.
Transmission of Yellow Fever Virus
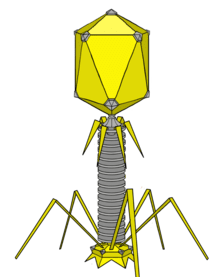
Yellow fever virus is an RNA virus that belongs to the genus Flavivirus. It is related to West Nile, St. Louis encephalitis, and Japanese encephalitis viruses. Yellow fever virus is transmitted to people primarily through the bite of infected Aedes or Haemagogus species mosquitoes. Mosquitoes acquire the virus by feeding on infected primates (human or non-human) and then can transmit the virus to other primates (human or non-human). People infected with yellow fever virus are infectious to mosquitoes (referred to as being “viremic”) shortly before the onset of fever and up to 5 days after onset.
Yellow fever virus has three transmission cycles: jungle (sylvatic), intermediate (savannah), and urban.
- The jungle (sylvatic) cycle involves transmission of the virus between non-human primates (e.g., monkeys) and mosquito species found in the forest canopy. The virus is transmitted by mosquitoes from monkeys to humans when humans are visiting or working in the jungle.
- In Africa, an intermediate (savannah) cycle exists that involves transmission of virus from mosquitoes to humans living or working in jungle border areas. In this cycle, the virus can be transmitted from monkey to human or from human to human via mosquitoes.
- The urban cycle involves transmission of the virus between humans and urban mosquitoes, primarily Aedes aegypti. The virus is usually brought to the urban setting by a viremic human who was infected in the jungle or savannah (Figure 1).

Symptoms, Diagnosis, & Treatment of yellow fever
The majority of people infected with yellow fever virus will either not have symptoms, or have mild symptoms and completely recover.
For people who develop symptoms, the time from infection until illness is typically 3 to 6 days.
Because there is a risk of severe disease, all people who develop symptoms of yellow fever after traveling to or living in an area at risk for the virus should see their healthcare provider. Once you have been infected, you are likely to be protected from future infections.
Symptoms of yellow fever
- Most people will not have symptoms.
- Some people will develop yellow fever illness with initial symptoms including:
- Sudden onset of fever
- Chills
- Severe headache
- Back pain
- General body aches
- Nausea
- Vomiting
- Fatigue (feeling tired)
- Weakness
- Most people with the initial symptoms improve within one week.
- For some people who recover, weakness and fatigue (feeling tired) might last several months.
- A few people will develop a more severe form of the disease.
- For 1 out of 7 people who have the initial symptoms, there will be a brief remission (a time you feel better) that may last only a few hours or for a day, followed by a more severe form of the disease.
- Severe symptoms include:
- High fever
- Yellow skin (jaundice)
- Bleeding
- Shock
- Organ failure
- Severe yellow fever disease can be deadly. If you develop any of these symptoms, see a healthcare provider immediately.
- Among those who develop severe disease, 30-60% die.
Diagnosis of yellow fever
- Yellow fever infection is diagnosed based on laboratory testing, a person’s symptoms, and travel history.
- More information on diagnostic testing is available on the For Healthcare Providers page.
Treatment of yellow fever
- There is no medicine to treat or cure infection from yellow fever.
- Rest, drink fluids, and use pain relievers and medication to reduce fever and relieve aching.
- Avoid certain medications, such as aspirin or other nonsteroidal anti-inflammatory drugs, for example ibuprofen (Advil, Motrin), or naproxen (Aleve), which may increase the risk of bleeding.
- People with severe symptoms of yellow fever infection should be hospitalized for close observation and supportive care.
- If after returning from travel you have symptoms of yellow fever (usually about a week after being bitten by an infected mosquito), protect yourself from mosquito bites for up to 5 days after symptoms begin. This will help prevent spreading yellow fever to uninfected mosquitoes that can spread the virus to other people.
Source:
CDC. Yellow fever vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59(RR-7):1–27.
CDC. Yellow fever vaccine booster doses: Recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(23):647–50.
CDC. Notes from the Field: Fatal Yellow Fever Vaccine–Associated Viscerotropic Disease — Oregon, September 2014. MMWR Morb Mortal Wkly Rep. 2015;64(10):279–281.
Barwick R. History of thymoma and yellow fever vaccination. Lancet. 2004;364(9438):936.
Cavalcanti DP, Salomao MA, Lopez-Camelo J, et al. Early exposure to yellow fever vaccine during pregnancy. Trop Med Int Health. 2007;12(7):833–7.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.