Urease test is used to detect and differentiate Enterobacteriaceae that produce urease enzymes from those that do not. The urease test is used to determine the ability of an organism to split urea, through the production of the enzyme urease.
Urease is an exoenzyme that hydrolyzes urea to produce ammonia and carbondioxide. Urease positive enterobacteria produce urease enzyme which has the ability to breakdown urea to ammonia (NH3) and carbon (IV) oxide (CO2).
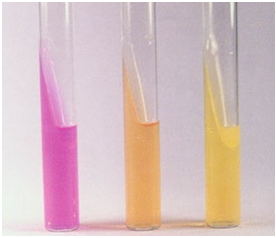
To test for urease production in bacteria, test isolates are cultured in a medium that contains urea and an indicator phenol red which changes colour from yellow to pink following the release of NH3 which turns the medium alkaline. Urease test can be performed in the laboratory using modified Christensen’s urea broth, a urease testing tablet or a urea agar medium.
The culture medium used for urease test include any urea medium, agar or broth; and any of these medium could be a sole medium or part of a panel like the motility indole urease (MIU) test medium that is used to determine the motility, indole production and urease production of a given bacterium. Proteus, Klebsiella and Providencia species are strong producers of urease enzymes.
PROCEDURE FOR UREASE TEST
- Prepare urea agar medium slant in a test tube according to manufacturer’s instruction. In the preparation, test tube(s) containing the citrate medium must be kept in slanting position in order to make a slope. Well prepared urea slant looks yellowish.
- Perform this test with a pure culture of the test isolate grown on a nutrient agar plate.
- Aseptically inoculate a speck or inoculum of the test isolate on urea agar medium slant by streaking.
- Incubate the slant(s) overnight at 37oC.
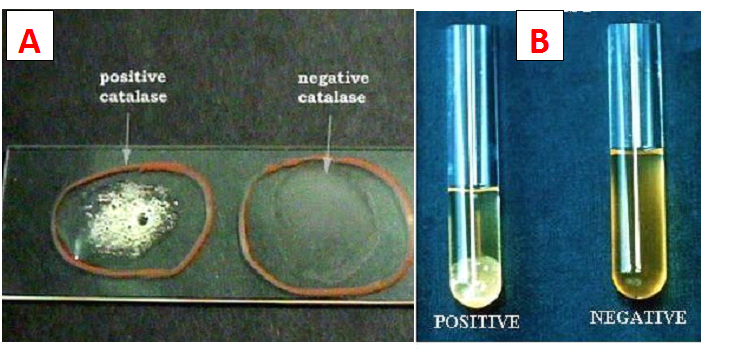
- Observe the slant for a pink colouration. The production of a pink colouration is indicative of a positive result (Figure 1). Absence of a pink colour shows a negative test result, and nonexistence of a urease producer.
References
Basic laboratory procedures in clinical bacteriology. World Health Organization (WHO), 1991. Available from WHO publications, 1211 Geneva, 27-Switzerland.
Beers M.H., Porter R.S., Jones T.V., Kaplan J.L and Berkwits M (2006). The Merck Manual of Diagnosis and Therapy. Eighteenth edition. Merck & Co., Inc, USA.
Biosafety in Microbiological and Biomedical Laboratories. 5th edition. U.S Department of Health and Human Services. Public Health Service. Center for Disease Control and Prevention. National Institute of Health. HHS Publication No. (CDC) 21-1112.2009.
Cheesbrough M (2010). District Laboratory Practice in Tropical Countries. Part I. 2nd edition. Cambridge University Press, UK.
Cheesbrough M (2010). District Laboratory Practice in Tropical Countries. Part 2. 2nd edition. Cambridge University Press, UK.
Collins C.H, Lyne P.M, Grange J.M and Falkinham J.O (2004). Collins and Lyne’s Microbiological Methods. Eight edition. Arnold publishers, New York, USA.
Disinfection and Sterilization. (1993). Laboratory Biosafety Manual (2nd ed., pp. 60-70). Geneva: WHO.
Garcia L.S (2010). Clinical Microbiology Procedures Handbook. Third edition. American Society of Microbiology Press, USA.
Garcia L.S (2014). Clinical Laboratory Management. First edition. American Society of Microbiology Press, USA.
Fleming, D. O., Richardson, J. H., Tulis, J. I. and Vesley, D. (eds) (1995). Laboratory Safety: Principles and practice. Washington DC: ASM press.
Dubey, R. C. and Maheshwari, D. K. (2004). Practical Microbiology. S.Chand and Company LTD, New Delhi, India.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.