Periodontitis is defined as the microbial infection of the periodontal membrane leading to pyorrhea, and resulting in the teeth falling out if left untreated. It is the inflammation of the periodontium. Periodontitis can occur from the penetration of the periodontal membrane by pathogenic bacteria or the activation of resident oral bacteria in the mouth. Prior to the development of periodontitis in an individual, there is usually a colonization of the subgingival regions of the tooth by specific groups of bacterial organisms.
The colonization of the subgingival regions leads to the release of several virulent factors including proteases and leukotoxins – which exacerbate the virulent nature of the colonizing bacteria. There is an outright response of the host’s immune system to this bacterial colonization of the subgingival regions of the teeth. However, the immune response to bacterial colonization is usually destructive in form; and this leads to the loss of periodontal tissues, thus causing periodontitis. The inflammation of the periodontal membrane or periodontium may assume different forms depending on the level of the bacterial infection.
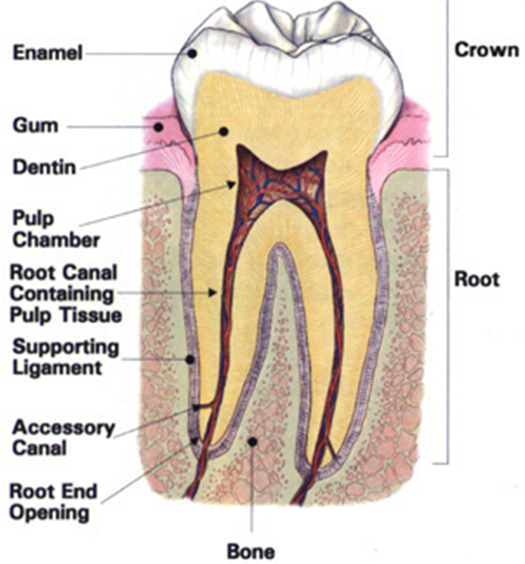
Periodontal membrane is the membranous covering around the teeth, and it can also be called periodontium. The periodontium includes the gum and bone portion of a tooth, and it is a usually site of attack by microbial organisms in the oral cavity including bacterial and fungal species. The inflammation that is associated with periodontitis in humans may be chronic or acute in occurrence; and the disease can by symptomatic or asymptomatic in form. Individuals with asymptomatic periodontitis may be unaware of the infection until tooth mobility sets in. But those with symptomatic periodontitis experiences tooth mobility; and there is a further destruction of the fibers of the periodontal ligament of individuals with symptomatic periodontitis.
Chronic periodontitis is usually slower in form and it is protracted. In chronic periodontitis, the destruction and loss of the affected tooth or teeth takes a slower pace. In chronic periodontitis, the degradation of the connective tissues surrounding and supporting the teeth gradually loses its protective function and the tooth starts to shake.
Acute periodontitis is usually characterized by an aggressive destruction of the tissues supporting the affected teeth. It occurs sporadically and does not take the protracted form that is usually experienced in chronic periodontitis. Periodontitis is a gum infection, initiated by specific bacteria that activate a series of inflammatory and immunologic changes leading to destruction of connective tissue and bone portions of the teeth.
As aforementioned, periodontitis can lead to the possible loss of the teeth especially when the affected tooth is left untreated. The periodontium or periodontal membrane of a tooth is made up of the gingivae (gum), cementum, periodontal ligament and the alveolar bone. Periodontitis is the most common chronic bacterial infection in adults; and adult periodontitis occurs when periodontitis stays for 5-10 years without any formal treatment. It is characterized by the outright destruction of the connective tissue attached to the teeth.
The destruction of the connective tissues of the bone coupled with the damage of the alveolar bone leads to the production of deeper pockets (holes) in the periodontium. Such holes contribute to the loss of the affected tooth as well as in the development of a possible secondary bacterial infection in affected individuals.
The outright destruction of the alveolar bone, halitosis and tooth mobility is some of the main clinical features of periodontitis. Several bacterial organisms are implicated as causative agents of periodontitis in humans. The major bacterial species that cause periodontitis in humans include Bacteroides gingivalis, B. intermedius, Bacillus gingivalis, Fusobacterium nucleatum, Streptococcus mileri, Treponema species and Eikenella corrodens. The major difference between gingivitis and periodontitis is that there is no tooth loss in the former but tooth loss is common in periodontitis. Periodontitis also occurs in adolescents or juveniles.
Juvenile periodontitis is normally associated among adolescents; and it usually starts from the first permanent molar and then gradually progresses to other parts of the juvenile’s teeth. Bacteriodes gingivalis, Capnocytophaga species, Actinobacillus species, and Eikenella corrodens are some of the major bacterial species implicated in causing juvenile periodontitis. Some of the major predisposing factors that cause periodontitis in humans include: the oral hygiene of the individual, age, trauma, anatomy of the teeth, and individual immunological factors.
Maintaining a good oral hygiene, doing scaling and polishing at dental clinics and using recommended mouth washes can help to prevent the disease. Surgery can be used to remove affected tooth; and chemotherapy which mainly involves the use of antibiotics can also be used for treating periodontitis. And tooth loss in individuals with periodontitis can also be replaced with an artificial tooth.
References
Barrett J.T (1998). Microbiology and Immunology Concepts. Philadelphia, PA: Lippincott-Raven Publishers. USA.
Beck, J. D., Slade, G. and Offenbacher, S. (2000). Oral disease, cardiovascular disease and systemic inflammation. Periodontol, 23, 110-20.
Beers M.H., Porter R.S., Jones T.V., Kaplan J.L and Berkwits M (2006). The Merck Manual of Diagnosis and Therapy. Eighteenth edition. Merck & Co., Inc, USA.
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA.
Champoux J.J, Neidhardt F.C, Drew W.L and Plorde J.J (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases. 4th edition. McGraw Hill Companies Inc, USA.
Davey M.E and O’toole G.A (2000). Microbial biofilms: from ecology to molecular genetics. Microbiol. Mol. Biol. Rev, 64, 847-867.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Jenstch, H., Pornowski, R., Kundi, G. and Gocke, R. (2003). Treatment of gingivitis with hyaluronan. J. Clin. Periodontol.,30, 159-164.
Mayooran B, Robin S and John R.T (2000). Dental caries is a preventable infectious disease. Aust. Dent. J, 45, 235-245.
Trahan L.X (1995). A review of its action on mutans streptococci and dental plaque–its clinical significance. Int. Dent. J, 45, 77-92.
Warren L (2008). Review of Medical Microbiology and Immunology. Tenth edition. McGraw Hill Companies Inc, USA.
Wilson B. A, Salyers A.A, Whitt D.D and Winkler M.E (2011). Bacterial Pathogenesis: A molecular Approach. Third edition. American Society of Microbiology Press, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.