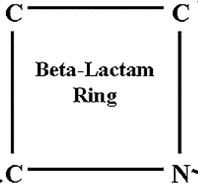
Aside penicillins and cephalosporins, other beta-lactam antibiotics used for clinical applications also exist. These beta-lactam antibiotics have expanded antibacterial activity, and they are often used to treat infections caused by bacterial pathogens that are resistant to the penicillins and cephalosporins.
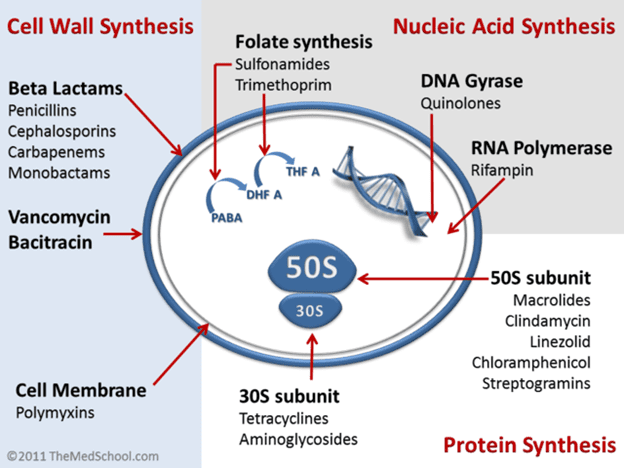
Antibiotics in this category are generally cell wall synthesis inhibitors, and they possess similar mechanisms of action like the penicillins and cephalosporins. They have broader spectrum of activity and are very effective against Gram positive and Gram negative bacteria. These other beta-lactam antibiotics and non-beta lactams that interrupt the synthesis of peptidoglycan in bacteria are shown below:
- Carbapenems e.g. imipenem, meropenem and ertapenem. Carbapenems are active against a wide variety of bacteria including Gram positive and Gram negative bacteria as well as against anaerobic bacteria. They have the broadest spectrum of antibacterial activity than all the other beta-lactam drugs including penicillins and cephalosporins. Carbapenems are clinically used to treat infections caused by multidrug resistant bacteria including those that produce ESBLs.
- Monobactams e.g. aztreonam. Aztreonam is effective for treating infections caused by Gram negative bacteria; and it is the drug of choice for patients who are allergic to penicillins or cephalosporins. Monobactams are least effective against Gram positive bacteria.
- Cephamycins, which areβ-lactamswitha wider antibacterial spectrum than the cephalosporins. They are more stable to beta-lactamase hydrolysis. Examples include cefotetan, cefmetazole and cefoxitin. The cephamycins are very similar to the cephalosporins and are sometimes classified as cephalosporins. Though naturally sourced from Streptomyces, cephamycins can now be produced synthetically.
- Glycopeptides e.g. vancomycin produced by Streptomyces species. Vancomycin is more effective against Gram positive bacteria than Gram negative organisms because the drug cannot penetrate the OM of the latter. The existence of vancomycin-resistant bacteria has compromised the clinical use of vancomycin. Vancomycin is not a beta-lactam drug like the penicillins even though they interrupt peptidoglycan synthesis in Gram positive bacteria.
- Bacitracin, a polypeptide antibiotic naturally synthesizedby Bacillus licheniformis. Bacitracin is mainly used for topical applications (e.g. for ointment) because of their very high toxicity which prohibittheir usage for systemic administration.They are not beta-lactam antibiotics but interfere with the synthesis of peptidoglycan in pathogenic bacteria.
Carbapenems, monobactams, bacitracin and the glycopeptides inhibit the synthesis of bacterial cell wall by interfering with the transpeptidation reaction (required for the formation of peptidoglycan or murein) the same way that the cephalosporins and penicillins operate in vivo.
References
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Axelsen P. H (2002). Essentials of Antimicrobial Pharmacology. Humana Press, Totowa, NJ.
Balfour H. H (1999). Antiviral drugs. N Engl J Med, 340, 1255–1268.
Beck R.W (2000). A chronology of microbiology in historical context. Washington, D.C.: ASM Press.
Chemotherapy of microbial diseases. In: Chabner B.A, Brunton L.L, Knollman B.C, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, McGraw-Hill; 2011.
Chung K.T, Stevens Jr., S.E and Ferris D.H (1995). A chronology of events and pioneers of microbiology. SIM News, 45(1):3–13.
Courvalin P, Leclercq R and Rice L.B (2010). Antibiogram. ESKA Publishing, ASM Press, Canada.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Hugo & Russell’s Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA. Pp.152-172.
Dictionary of Microbiology and Molecular Biology, 3rd Edition. Paul Singleton and Diana Sainsbury. 2006, John Wiley & Sons Ltd. Canada.
Drusano G.L (2007). Pharmacokinetics and pharmacodynamics of antimicrobials. Clin Infect Dis, 45(suppl):89–95.
Engleberg N.C, DiRita V and Dermody T.S (2007). Schaechter’s Mechanisms of Microbial Disease. 4th ed. Lippincott Williams & Wilkins, Philadelphia, USA.
Finch R.G, Greenwood D, Norrby R and Whitley R (2002). Antibiotic and chemotherapy, 8th edition. Churchill Livingstone, London and Edinburg.
Ghannoum MA, Rice LB (1999). Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev, 12:501–517.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.