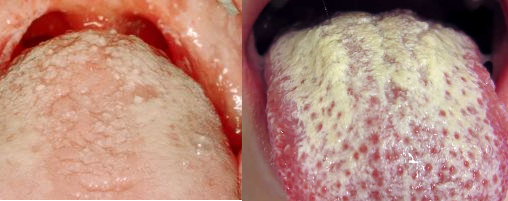
Oral thrush (oral candidiasis) is a localized fungal infection caused by C. albicans in the oral cavity of humans such as the tongue, lips and gums. Oral thrush is a fungal infection of the mouth; and thrush or oral thrush is an infection of the mouth caused by the Candida fungus which is a yeast cell.
Oral candidiasis is characterized by the formation of whitish mucoid plaques on the mucous membranes of the mouth; and the infection is known as endogenous mycoses because the causative agent (C. albicans) is part of the normal flora of the human body, found especially in the gut, mouth and respiratory tract. Mycoses due to Candida species in humans occur following the suppression of the body’s immunity (e.g. in HIV/AIDS individuals).
Other predisposing factors such as prolonged antibiotic usage and the use of immunosuppressive drugs are other risk factors to the development of oral candidiasis in humans. Oral candidiasis is strictly opportunistic mycoses that develop in people with poor immunity. The disease can also occur in newborns delivered via Candida infected vagina.
It is noteworthy that candidiasis in newborns is not an endogenous fungal infection but a contracted disease that occurs in infants from mother to child especially when the birth canal or vagina is heavily contaminated with C. albicans. Vulvovaginitis is a common Candida infection in pregnant women, and it is usually characterized by itching and irritation and discharge from the vagina of affected women.
Oral thrush is one type of candidiasis in humans. Other clinical forms of candidiasis include vaginal candidiasis, cutaneous candidiasis, mucosal and mucocutaneous candidiasis and systemic candidiasis. Other yeasts of medical importance aside Candida species include Saccharomyces species, Torulopsis speciesand Cryptococcus species. Candida albicans is responsible for most of the candidiasis episodes in humans. However, other Candida species such as C. kruzei, C. tropicalis, C. parapsilosis and C. guillermondii amongst other Candida species can also cause mild infections in humans.
Candida infection is not limited to the mouth; and thus, it can occur in other parts of the body as including the vagina of women. Small amounts of the Candida albicans are present in the mouth, digestive tract, and skin of most healthy people; and this beneficial fungus are normally kept in check by other bacteria (which are normal microflora) in the body.
However, stress, diseases and the use of medications such as antibiotics, birth control pills and corticosteroids can disturb the natural balance of the fungus in the body. This will cause C. albicans to grow out of control and cause thrush in the affected host. The use of such medications weakens the immune system and cause Candida to thrive. Nystatin, fluconazole, amphotericin B and itraconazole can be used to treat thrush.
References
Anaissie E.J, McGinnis M.R, Pfaller M.A (2009). Clinical Mycology. 2nd ed. Philadelphia, PA: Churchill Livingstone Elsevier. London.
Beck R.W (2000). A chronology of microbiology in historical context. Washington, D.C.: ASM Press.
Black, J.G. (2008). Microbiology: Principles and Explorations (7th ed.). Hoboken, NJ: J. Wiley & Sons.
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA.
Brown G.D and Netea M.G (2007). Immunology of Fungal Infections. Springer Publishers, Netherlands.
Calderone R.A and Cihlar R.L (eds). Fungal Pathogenesis: Principles and Clinical Applications. New York: Marcel Dekker; 2002.
Chakrabarti A and Slavin M.A (2011). Endemic fungal infection in the Asia-Pacific region. Med Mycol, 9:337-344.
Champoux J.J, Neidhardt F.C, Drew W.L and Plorde J.J (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases. 4th edition. McGraw Hill Companies Inc, USA.
Chemotherapy of microbial diseases. In: Chabner B.A, Brunton L.L, Knollman B.C, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, McGraw-Hill; 2011.
Chung K.T, Stevens Jr., S.E and Ferris D.H (1995). A chronology of events and pioneers of microbiology. SIM News, 45(1):3–13.
Germain G. St. and Summerbell R (2010). Identifying Fungi. Second edition. Star Pub Co.
Ghannoum MA, Rice LB (1999). Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev, 12:501–517.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Larone D.H (2011). Medically Important Fungi: A Guide to Identification. Fifth edition. American Society of Microbiology Press, USA.
Levinson W (2010). Review of Medical Microbiology and Immunology. Twelfth edition. The McGraw-Hill Companies, USA.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of Microorganisms, 12th edition. Pearson Benjamin Cummings Inc, USA.
Mahon C. R, Lehman D.C and Manuselis G (2011). Textbook of Diagnostic Microbiology. Fourth edition. Saunders Publishers, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.