Genetic resistance of microbes to antibiotics is due to a chromosomal mutation in the bacterial DNA or acquisition of antibiotic resistance genes on plasmids or transposons from other bacteria. Bacteria are extremely ingenious in becoming resistant to antibiotics directed towards them because they are able to regulate their drug resistance genes over time.
This is often exacerbated by prior antibiotic usage especially irrational drug use. In this case where bacteria regulate their drug resistance genes, antibiotics used against them for treatment is inadvertently rendered useless in vivo. The genetic basis for antibiotic resistance may include: the acquisition and further expression of new DNA by horizontal gene transfer or mutations in cellular genes or acquired genes that alter antibiotic target sites on the bacteria.
The genetic alterations (mutation) mediate a diversity of biochemical mechanisms of resistance that benefits the bacteria, and in turn makes the antibiotic less efficacious in vivo. These mechanisms may include:
- Enzymatic inactivation of the antibiotic.
- Target substitutions, amplification or modifications bypassing the binding of the antibiotic, or reducing the affinity of the bacteria for the drug.
- Barriers such as efflux pumps which reduce the access of the antibiotic to the target site of the bacteria.
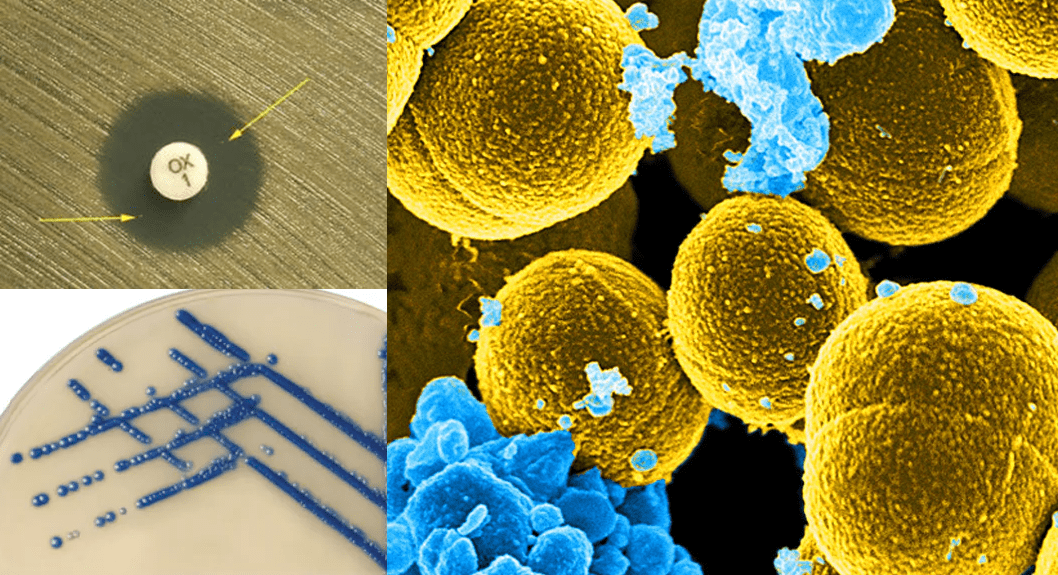
Antibiotic – resistant bacteria owe their drug insensitivity and ingenuity in developing resistance against our therapeutic regimens to some resistance genes which they harbor or possess. These resistance genes confer on these pathogens the ingenuity to evade the antimicrobial onslaught of antibiotics directed towards them. It is these genes that resistant bacteria transfer to non-resistant susceptible strains, thus compounding the problem of antibiotic resistance.
There are several molecular mechanisms through which pathogenic bacteria can become resistant to the onslaught of an antimicrobial action either in vivo or in vitro. The target organism’s uses these mechanisms to reduce the intracellular concentration of the drug required to either kill or inhibit the growth of the microbe. The organism eventually becomes resistant to the agent because the required concentration required to exhibit antimicrobial activity has not been achieved.
Though the prior usage of antibiotic can spur resistance in an organism, but this scenario is worsened when antimicrobial agents particularly antibiotics meant for human medicine are used for several non-clinical purposes such as in agriculture and for livestock and animals production. The irrational use of antibiotics in the community as well as the high intensity of some high profile antibiotics in the hospital are other predisposing factors that allow drug-resistant microorganisms to emerge and spread in both the community and hospital environment. When resistance occurs, sensitive or susceptible bacteria can become resistant to several antimicrobial agents in many ways.
It is noteworthy that some of the antibiotics that now exist and are used in clinical medicine have specific target site on the bacteria which they bind and interfere with their normal metabolism. In such scenarios the target organism becomes incapacitated and dies in some cases. But some microorganisms like the mycoplasmas and other wall-less bacteria are naturally resistant to some class of antibiotics such as the penicillins which are beta-lactam because the drug (i.e. the beta-lactams) only target the cell wall of bacteria; and thus such agents are useless when used for bacteria without cell wall. New drug targets should be discovered in pathogenic bacteria in order to contain the growing rates of resistance amongst pathogenic microorganisms. Some of the notable ways via which pathogens develop resistance to antibiotics are as follows:
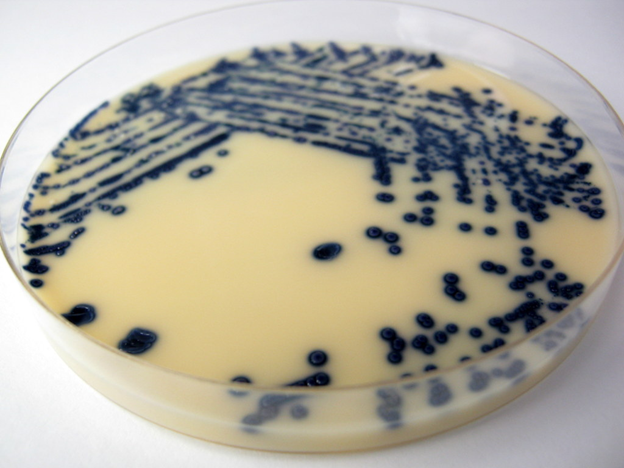
- Pathogenic bacteria produce enzymes that modify or inactivate antibiotics in vivo. Typical amongst this is the beta-lactamase enzymes of which there are now multidrug degrading-enzymes such as the ESBLs, MBLs and AmpC enzymes which render a large pool of antibiotics inefficacious. These enzymes are now widespread and they possess serious clinical threat in the hospital.
- Alteration or genetic mutation in the active sites of microorganisms can cause the efflux pump of the microbe to flush out the entry of antibiotics in order to prevent there intracellular accumulation.
- Modification of the drug target sites on the pathogen can make the drug less effective because it is only when they bind that they can unleash their antimicrobial activity.
- Pathogenic bacteria can also acquire resistance genes from resistant organisms in their environment. The incorporation of such resistance genes transforms the recipient susceptible bacteria to become a drug-resistant organism.
References
Alberts B, Lewis J, Raff M, Johnson A and Roberts K (2002). Molecular Biology of the Cell. Taylor and Francis, Inc, London, UK.
Das H.K (2008). Textbook of Biotechnology. Third edition. Wiley-India ltd., New Delhi, India.
Dictionary of Microbiology and Molecular Biology, 3rd Edition. Paul Singleton and Diana Sainsbury. 2006, John Wiley & Sons Ltd. Canada.
Friedberg EC, Walker GC and Siede WM (1995). DNA Repair and Mutagenesis. Washington, DC, USA: ASM Press.
Lederberg J (editor): Encyclopedia of Microbiology, 4 vols. Academic Press, 1992.
Lodish H, Berk A, Matsudaira P, Kaiser C.A, Kreiger M, Scott M.P, Zipursky S.L and Darnell J (2004). Molecular Cell Biology. Fifth edition. Scientific American Books, Freeman, New York, USA.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of Microorganisms, 12th edition. Pearson Benjamin Cummings Inc, USA.
Nelson, David L.; Cox, Michael M. (2005). Lehninger Principles of Biochemistry (4th ed.). New York: W.H. Freeman.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3d ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Tamarin Robert H (2002). Principles of Genetics. Seventh edition. Tata McGraw-Hill Publishing Co Ltd, Delhi.
Twyman R.M (1998). Advanced Molecular Biology: A Concise Reference. Bios Scientific Publishers. Oxford, UK.
Weaver R.F (2005). Molecular Biology. Third edition. McGraw-Hill Publishers, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.