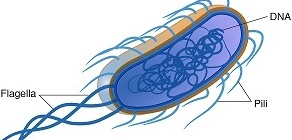
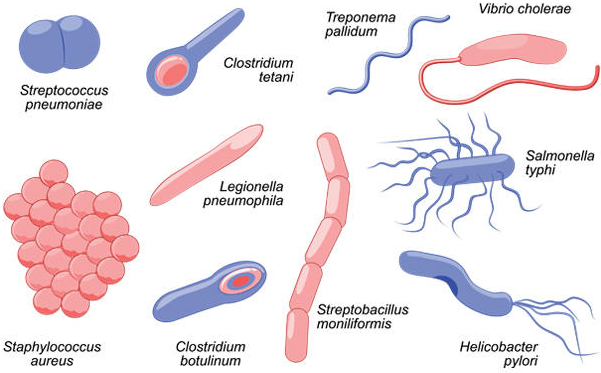
Escherichia coli is a facultative, enteric, Gram-negative, motile/flagellated, and lactose-fermenting rod that occur in the genus Escherichia and family Enterobacteria or Enterobacteriaceae. Enterobacteriaceae are bacteria that naturally exist in the intestinal tract of animals and humans, and also found in water and soil. Because the natural habitat of E. coli is the intestinal tract of humans (animals inclusive), it is therefore used as an indicator of the feacal contamination of drinking water and water used for other domestic and industrial purposes. As a baseline, 100 ml of drinking water must not contain any trace of E. coli.
While most enteric Gram-negative bacteria such as Shigella and Salmonella are important and regular human pathogens, E. coli are members of the normal intestinal flora and may only cause disease by chance. Basically, E. coli causes pathological conditions in humans when they become transient (i.e. when they leave their normal site in the intestine to tissues or parts of the body that are outside the intestines). It is noteworthy that all bacteria in the Enterobacteriaceae family are also called coliforms. A coliform is a Gram-negative non-sporulating facultative rod that ferments sugars (such as glucose and lactose) to produce gas within 48 h at 35oC.
The term coliform can also be used interchangeably with commensals. Though E. coli is a less common human pathogen, it is the most common cause of uncomplicated cystitis in man. Cystitis is a bacterial infection that occurs when feacal bacterial flora (e.g. E. coli) gains entry into the urethra and bladder of normal or healthy individuals. Pathogenic strains of E. coli are the commonest and leading causes of urinary tract infections (UTIs) in man, and they have also been implicated in other diseases such as bacteraemia, diarrheal diseases and sepsis.
For example, E. coli O157:H7 is an E. coli strain reserved in cattle/cow but causes haemorrhagic colitis, a zoonotic disease in man through the feacal-oral route. Note: ‘O’ stands for cell wall antigen while ‘H’ stands for flagella antigen. The capsular antigen of bacteria (e.g. Klebsiella species) is often represented with the alphabet “K”. E. coli is also amongst the top pathogens isolated from postsurgical wounds. In effect, E. coli is more of an opportunistic pathogen than a true pathogen, and its pathogenic strains are notorious in causing nosocomial (hospital-acquired) infections. Biochemically, E. coli are indole positive, haemolytic on blood agar and they ferment sugars to produce gas.
PATHOGENESIS OF ESCHERICHIA COLI INFECTION
E. coli is the most common normal flora of the intestinal tract of humans, and they can also be found in the genital tract and upper respiratory tracts in traces. The presence of pathogenicity islands (acquired foreign DNA) in the genome of enteropathogenic E. coli enhances the pathogenicity and/or virulence of the organism. Infections resulting from E. coli occur occasionally and this has been attributable to the relocation of the bacteria from its normal location in the intestine to other extra-intestinal sites. E. coli causes UTI, diarrheal diseases, meningitis, wound infections and peritonitis. They produce various types of toxins including shiga toxin, labile toxin, stable toxin amongst others; and these help to increase their virulence in the host cells.
Though E. coli is implicated in a handful of human infections when they have the opportunity, diarrheal diseases and UTIs are amongst the two most important infections that characterize the majority of hospital visits across the world. Based on their virulence, there are basically five groups of E. coli-associated diarrheal diseases. Urinary tract infections caused by E. coli usually arise from the entry of uropathogens into the bladder. Uropathogens can gain entry into the human bladder through sexual intercourse or some minor strain experienced during sexual activity.
Urinary tract infections (UTIs) are caused by the presence and growth of bacteria anywhere in the urinary tract system including the kidney, bladder and the urethra. Most cases of UTIs are asymptomatic but some are symptomatic and may present with some clinical signs and symptoms such as increased frequency of urination, dysuria and haematuria (i.e. blood in urine). UTIs affects either the upper urinary tract system (kidney and ureter) or the lower urinary tract system (the bladder and the urethra) of both males and females. However, UTIs are common health-associated infections in women than in men due to the shortness of the female urethra (which is about 1.5 inches) compared to that of their male counterparts (which is about 8 inches).
This natural anatomical difference in the urethra of males and females makes the contamination of the female’s urinary tract system from the external genitalia almost unavoidable. The female urethra is particularly prone to bacterial infection or invasion following the migration of pathogenic microorganisms from the anus or vagina. Pregnancy is another predisposing factor that increases the risk of acquiring a UTI. In pregnancy, physiological changes in the urogenital tract of expectant mothers increase their potential for pathogenic colonization by microbes such as E. coli that may eventually result to a UTI. Thus pregnant women are at a very high risk of acquiring a UTI beginning from week 6 through week 24 of their pregnancy than non-pregnant women.
The anatomical positioning of the uterus (womb) during pregnancy (which allows it to overlie the bladder and increase urine retention in the organ) coupled with possible poor hygiene and hormonal changes that occur during pregnancy makes it probable for a UTI to occur more in pregnant women than in non-expectant mothers. The use of anti-sperm agents such as spermicides also increases the risk for a UTI in women (pregnant ones inclusive). The ability of E. coli to produce a UTI is also associated with the virulence of the organism such as its ability to produce toxins and having appendages (e.g. pili and fimbria) that allows it to attach firmly to epithelial surfaces in the body.
PATHOGENIC STRAINS OF ESCHERICHIA COLI THAT CAUSES DIARRHEAL
DISEASES IN MAN
ENTEROPATHOGENIC E. COLI (EPEC)
EPEC strains causes diarrhea in infants and children in developing countries. EPEC strains adhere strictly to the epithelial cells of the intestines by means of an adhesion molecule and start proliferating. They cause lesions known as effacing or attaching-effacing lesions that affects the microvilli of the intestines, and this lead to profuse and prolonged diarrhea in infants. Vomiting can also be accompanied in an EPEC strain infection. The diarrhea caused by EPEC strains is generally self-limiting and but can be chronic and last longer in the infected children. The mode of transmission of this type of E. coli-associated diarrheal disease is via the feacal-oral route.
ENTEROTOXIGENIC E. COLI (ETEC)
ETEC strains are the main causative agents of traveler’s diarrhea in people visiting developing countries. It causes watery diarrhea in both infants and adults. ETEC strains produce a variety of enterotoxins that are responsible for the watery diarrhea they produce in their host. The enterotoxins (which are heat-stable and heat-labile in nature) bind to the epithelial cells of the intestines where they stimulate guanylate cyclase that activates the production of cyclic guanosine monophosphate (cGMP). This action mediates the inhibition of sodium ions (Na+) and stimulates the secretion of chloride ions (Cl–) and/or electrolytes and water into the lumen of the small intestine that finally result into watery diarrhea. The mode of transmission of this type of E. coli-associated diarrheal disease is via the feacal- oral route especially through the consumption of foods contaminated with human feaces.
ENTEROHAEMORRHAGIC E. COLI (EHEC)
EHEC strains are the causative agents of haemorrhagic colitis (a life-threatening bloody diarrhea), and they mainly affect the colon (large intestine) unlike other pathogenic strains of E. coli that attack solely the small intestines. They cause severe abdominal pain followed by bloody diarrhea and haemolytic uraemic syndrome (HUS) in humans. EHEC strains produce verotoxins (a shiga-like toxin) and are sometimes called verocytotoxin-producing E. coli (VTEC) because their toxin is cytotoxic on Vero cells (that originated from kidney cells of African green monkeys) in tissue cultures.
Consumption of food stuffs such as beef and other meat products from animals colonized by the bacteria are the main source of acquiring the pathogen. Spinach and unpasteurized fruit juices can also aid in the transmission of EHEC strains. EHEC disease (bloody diarrhea) is a disease of the developed countries. It occurs at a low frequency in developing countries. E. coli 0157:H7 serotype is a major form of EHEC strains as both are genetically related. The mode of transmission of this type of E. coli-associated diarrheal disease is via the feacal-oral route.
ENTEROINVASIVE E. COLI (EIEC)
EIEC strains cause E. coli-associated dysentery that resembles shigellosis. Shigellosis is caused by Shigella dysenteriae.Though EIEC infection may occur worldwide, children under the age of 5 years old and who live in developing countries are mostly affected by the disease.EIEC is toxigenic (i.e. it produces enterotoxins), and they penetrate the colonic mucosa and/or epithelial cells of the intestine where they cause inflammatory ulcerations that result in dysentery. The stool of infected patients is usually accompanied with blood, mucous, and pus cells. Contaminated food and water are the main source of acquiring the EIEC infections. The mode of transmission of this type of E. coli-associated diarrheal disease is via the feacal-oral route.
ENTEROAGGREGATIVE E. COLI (EAEC)
EAEC stains are the causative agents of food-borne disease in developed countries and chronic and acute diarrhea in people living in developing countries. They cause vomiting and watery diarrhea in infants and children living in developing nations. EAEC strains are notorious in adhering tightly to the intestinal mucosa of its human host to form biofilms or aggregates of bacterial cells. This type of E. coli-associated diarrhea is often associated with neonatal-nurseryoutbreaks in hospital settings. The mode of transmission of this type of E. coli-associated diarrheal disease is via the feacal-oral route.
LABORATORY DIAGNOSIS OF ESCHERICHIA COLI INFECTION
The laboratory diagnoses of E. coli-associated diarrheal diseases are mainly based on microscopy and isolation/culture of the infecting pathogen from clinically important specimens. Blood, urine, stool, and pus are some of the specimens obtained for laboratory analysis. A mid-stream urine (MSU) is required to diagnose UTI caused by E. coli in the laboratory.
Bacterial counts of E. coli less than 103 colony forming unit (CFU) per ml of urine indicate contamination while counts above 105 CFU/ml of urine are a strong indication of E. coli infection (i.e. significant bacteriuria). E. coli grow on MacConkey agar to produce smooth pink colonies (Figure 1), blood agar (to produce mucoid and haemolytic colonies for some strains), cystein lactose electrolyte deficient (CLED) medium (to produce yellow colonies) and on Hektoen enteric agar, XLA (to produce yellow colonies).
It also grows on triple sugar iron agar (TSIA) or Kligler iron agar (KIA) where some strains of E. coli produce gas (hydrogen sulphide, H2S) and acid. Sorbitol MacConkey agar is specifically used to screen for E. coli O157:H7 strain. Biochemically, E. coli strains are lactose fermenters, indole positive, lysine decarboxylase (LDC) positive, and they reduce nitrate to nitrite in dipstick analysis of urine test. Molecular detection techniques for prompt identification of E. coli strains include the use of PCR and DNA probes.

IMMUNITY TO ESCHERICHIA COLI INFECTION
There is no long-lasting immunity associated with E. coli-associated infections even though some appreciable levels of specific and non-specific resistance may be mounted during the onset of the disease. However, there is low incidence of the disease in breast-fed infants, thus underscoring the protective function of the maternal antibody transferred via breast milk.
TREATMENT OF ESCHERICHIA COLI INFECTION
Most cases of gastroenteritis caused by bacteria in the Enterobacteriaceae family (E. coli in particular) are self-limiting and often heal without any antibacterial therapy. Since E. coli-associated diarrheal diseases are often accompanied with the loss of fluids and electrolytes from the body, treatment and management of the disease should be started with fluid and electrolyte replacement. Administration of oral-rehydration therapy (containing specific amount of salt, sugar and water) to counter the possible dehydration in the diarrhea patient is the best form of supportive therapy because it returns the affected individuals to a normal fluid and electrolyte of the body.
Though some strains of E. coli may be resistant to some antibiotics, sulphamethoxazole-trimethoprim, doxycycline, fluoroquinolones, cephalosporins and aminoglycosides still have remarkable antibacterial effect on the pathogen. But the physician’s choice of using any of these agents should be guided by the susceptibility test results for each patient’s E. coli in order to reduce the emergence of resistance and guarantee appropriate treatment.
PREVENTION AND CONTROL OF ESCHERICHIA COLI INFECTION
The presence of E. coli in drinking water and water meant for other domestic or industrial purposes is enough indication of feacal contamination of the water source from either sewage or human feaces (especially in places where people defecate in water). Food meant for human consumption becomes contaminated with the pathogen when such water sources are used for either food processing or food contamination. Thus, the prevention of E. coli-associated diarrheal diseases involves avoiding the consumption of contaminated water and food.
Travelers or tourists visiting tropical countries should ensure that they only eat properly cooked food and drink only bottled and well disinfected water. Uncertain fruits, vegetables and water should be avoided as much as possible. People working in hospital facilities, clinics and other medical establishments should imbibe strict or good personal hygiene such as hand washing since E. coli and other enteric bacteria are opportunistic pathogens that can easily be transmitted from one person to another or from one body part to another where they cause infection.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.