Key facts about Buruli ulcer
- Buruli ulcer is a chronic debilitating disease caused by an environmental Mycobacterium ulcerans.
- It often affects the skin and sometimes bone and can lead to permanent disfigurement and long-term disability.
- At least 33 countries with tropical, subtropical and temperate climates have reported Buruli ulcer in Africa, South America and Western Pacific regions.
- The mode of transmission is not known and there is no prevention for the disease.
Buruli ulcer, caused by Mycobacterium ulcerans, is a chronic debilitating disease that affects mainly affects the skin and sometimes bone. The organism belongs to the family of bacteria that causes tuberculosis and leprosy, which provides an opportunity for collaboration with these disease programmes. However, M. ulcerans is an environmental bacterium and produces unique toxin – mycolactone. The mode of transmission to humans remains unknown. Currently, early diagnosis and treatment are crucial to minimizing morbidity, costs and prevent long-term disability.
Scope of the problem
Buruli ulcer has been reported in 33 countries in Africa, the Americas, Asia and the Western Pacific. Most cases occur in tropical and subtropical regions except in Australia, China and Japan. Out of the 33 countries, 14 regularly report data to WHO.
The annual number of suspected Buruli ulcer cases reported globally was around 5000 cases up until 2010 when it started to decrease until 2016, reaching its minimum with 1961 cases reported. Since then, the number of cases has started to rise again every year, up to 2713 cases in 2018. In 2020 1258 cases were reported compared with 2271 cases in 2019. The reduction in 2020 could be linked to the impact of Covid-19 on active detection activities.
Transmission of Buruli ulcer (Mycobacterium ulcerans infection)
Mycobacterium ulcerans grows at temperatures between 29–33 °C (Mycobacterium tuberculosis grows at 37 °C) and needs a low (2.5%) oxygen concentration. The organism produces a unique toxin – mycolactone – which causes tissue damage and inhibits the immune response.
The exact mode of transmission of M. ulcerans is still unknown.
Signs and symptoms of Buruli ulcer (Mycobacterium ulcerans infection)
Buruli ulcer often starts as a painless swelling (nodule), a large painless area of induration (plaque) or a diffuse painless swelling of the legs, arms or face (oedema). The disease may progress with no pain and fever. Without treatment or sometimes during antibiotics treatment, the nodule, plaque or oedema will ulcerate within 4 weeks. Bone is occasionally affected, causing deformities.
The disease has been classified into three categories of severity: Category I single small lesion (32%), Category II non-ulcerative and ulcerative plaque and oedematous forms (35%) and Category III disseminated and mixed forms such as osteitis, osteomyelitis and joint involvement (33%).
Lesions frequently occur in the limbs: 35% on the upper limbs, 55% on the lower limbs, and 10% on the other parts of the body. Health workers should be careful in the diagnosis of Buruli ulcer in patients with lower leg lesions to avoid confusion with other causes of ulceration such as diabetes, arterial and venous insufficiency lesion.
Diagnosis of Buruli ulcer (Mycobacterium ulcerans infection)
In most cases, experienced health professionals in endemic areas can make a reliable clinical diagnosis but training is essential.
Other conditions should be excluded from the diagnosis, including tropical phagedenic ulcers, chronic lower leg ulcers due to arterial and venous insufficiency (often in elderly populations), diabetic ulcers, cutaneous leishmaniasis, extensive ulcerative yaws and ulcers caused by Haemophilus ducreyi.
Early nodular lesions are occasionally confused with boils, lipomas, ganglions, lymph node tuberculosis, onchocerciasis nodules or deep fungal subcutaneous infections.
In Australia, papular lesions may initially be confused with an insect bite.
Cellulitis may look like oedema caused by M. ulcerans infection but in the case of cellulitis, the lesions are painful and the patient is ill and febrile.
HIV infection complicates the management of the patient, making clinical progression more aggressive and resulting in poor treatment outcomes.
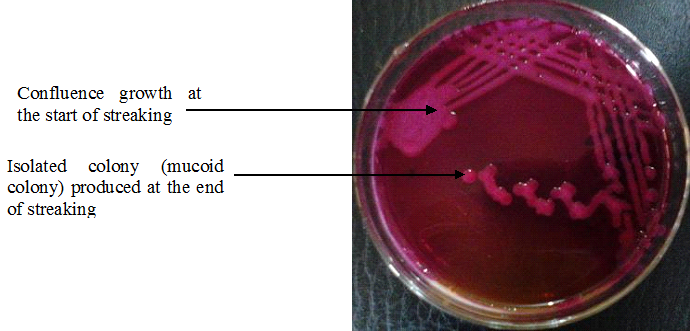
Four standard laboratory methods can be used to confirm Buruli ulcer: IS2404 polymerase chain reaction (PCR), direct microscopy, histopathology and culture.
In 2019, WHO established the Buruli ulcer Laboratory Network for Africa1 to help strengthen PCR confirmation in 9 endemic countries in Africa. 13 laboratories participate in this network – supported by the American Leprosy Missions, Anesvad, Raoul Follereau Foundation and the Foundation for Innovative Diagnostic and coordinated by the Pasteur Center of Cameroon.
Treatment of Buruli ulcer (Mycobacterium ulcerans infection)
Treatment consists of a combination of antibiotics and complementary treatments. Treatment guidance for health workers can be found in the WHO publication Treatment of mycobacterium ulcerans disease (Buruli ulcer).
A recent study suggests the combination of rifampicin (10 mg/kg once daily) and clarithromycin (7.5 mg/kg twice daily) is now the recommended treatment.
In Australia, a combination of rifampicin (10 mg/kg once daily) and moxifloxacin (400 mg once daily) is routinely used with good results but its effectiveness has not been proven.
Telacebec is a new anti-tuberculous drug developed by a Korean company Qurient.2 The drug has demonstrated extreme potent activity against Mycobacterium ulcerans in animal studies34, reducing treatment duration from 8 to 2 weeks. In January 2021, the US Food and Drug Administration granted orphan drug designation (ODD) to Telacebec, a Buruli ulcer treatment.5 A clinical trial is being planned to evaluate the drug in patients.
Interventions such as wound and lymphoedema management and surgery (mainly debridement and skin grafting) are used to speed up healing, thereby shortening the duration of hospitalization. Physiotherapy is needed in severe cases to prevent disability. Those left with disability require long-term rehabilitation. These same interventions are applicable to other neglected tropical diseases, such as leprosy and lymphatic filariasis.
Prevention and control of Buruli ulcer (Mycobacterium ulcerans infection)
There are currently no primary preventive measures for Buruli ulcer. The mode of transmission is not known. Bacillus Calmette–Guérin (BCG) vaccination appears to provide limited protection.
The objective of Buruli ulcer control is to minimize the suffering, disabilities and socioeconomic burden. Early detection and antibiotic treatment are the cornerstones of the control strategy.
WHO response to Buruli ulcer (Mycobacterium ulcerans infection)
WHO provides technical guidance, develops policies, and coordinates control and research efforts. WHO brings together all major actors involved in Buruli ulcer on a regular basis to share information, coordinate disease control and research efforts, and monitor progress.
WHO supports work towards three research priorities:
- understand the mode of transmission
- develop rapid diagnostic tests
- establish best-case antibiotic treatments.
Source:
www.who.int/news-room/fact-sheets/detail/buruli-ulcer-(mycobacterium-ulcerans-infection)
Discover more from #1 Microbiology Resource Hub
Subscribe to get the latest posts to your email.