Antibacterial agents are specifically chemical agents that kill or inhibit the growth of pathogenic bacteria. They are generally known as antibiotics. Antibiotics are complex chemical and natural substances that are secreted by some group of microorganisms (especially fungi, protozoa and bacteria), and which have the ability to either kill or inhibit the growth of other microbes. Prior to the manufacture of synthetic and semi-synthetic antibiotics, antibiotics were formerly defined as substances produced by microorganisms and which killed or inhibited the growth of other microbes. Though there is no census to the actual definition of antibiotics; to be all encompassing, an “antibiotic” can best be defined as a substance produced by a microorganism (wholly or partly by chemical synthesis) which in low or defined concentrations have the ability to kill or inhibit the growth of other susceptible microbes.
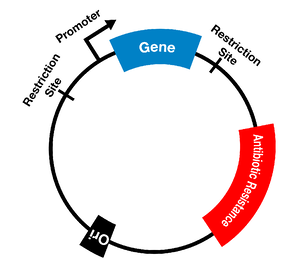
The term antibiotics can synonymously be used with antimicrobial agents. Penicillin and tetracycline are examples of some naturally synthesized antibiotics produced by Penicillium species and Streptomyces species respectively. However, some of the available antibiotics are now synthesized by chemical processes using derivatives from their natural or original sources. Antibiotics are either used topically or systemically; and their primary function is to kill or inhibit the growth of invading pathogenic bacteria in humans. Antibiotics are secondary metabolites produced by bacteria. They destabilize certain metabolic process of their target organisms, and thus restore the health of the affected host. It is noteworthy that the bacteria that produce these antimicrobial agents remain resistant to their own lethal substance, but they are susceptible to the antibiotics secreted by other bacterial species or microbes.
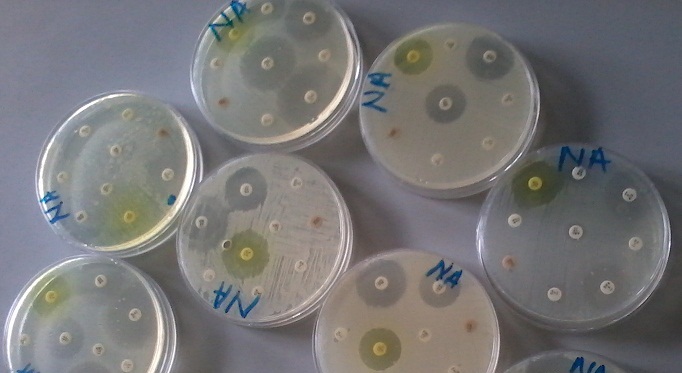
Antibiotics can be classified as cell wall inhibitors; protein synthesis inhibitors; anti-metabolites or nucleic acid synthesis inhibitors depending on the mechanism of action of the drug. Other classes of antibiotics also target the cytoplasmic or plasma membrane of the bacterial cell. Different antibiotics have different modes or mechanisms of action, owing to the nature of their structure and degree of affinity to certain target sites within bacterial cells. Antimicrobial agents and/or antibiotics are critical for the selective isolation of microbes from both clinical and environmental samples. Antibiotics are incorporated into culture media including bacteriological and mycological media to act as inhibitory substances to the growth of some unwanted organisms (Table 1). They are mainly used in culture media generally known as selective culture media (culture media that allow some organisms to grow while inhibiting the growth of unwanted microbes).
Table 1. Antibiotics used in selective culture media as inhibitory substances
| Antibiotics | Spectrum of activity | Mechanism of action |
| Penicillin | Active on Gram positive and Gram negative bacteria, but mostly active on the former | Inhibits bacterial cell wall synthesis by preventing the formation of peptidoglycan, a key cell wall component |
| Tetracycline | Broad spectrum agent | Inhibits protein synthesis in bacteria by binding to the 30S ribosomal subunit |
| Novobiocin | Active on Gram-negative bacteria | Inhibits bacterial DNA synthesis |
| Chloramphenicol | Broad spectrum agent | Inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit |
| Streptomycin | Broad spectrum agent | Inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit |
| Erythromycin | Mostly active on Gram positive bacteria | Inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit |
| Polymyxin | Active on Gram negative bacteria especially Pseudomonas species | Disrupts cell membrane of bacteria |
| Rifampicin | Active on Gram positive bacteria | Inhibit bacterial RNA synthesis by inhibiting bacterial DNA-dependent RNA polymerase enzyme |
| Nalidixic acid | Active on Gram negative bacteria | Inhibits bacterial DNA synthesis by interfering with the activity of DNA gyrase |
| Trimethoprim | Broad spectrum agent | Inhibit purine synthesis in bacteria |
| Cycloheximide | Active on saprophytic fungi | Inhibit protein biosynthesis in eukaryotic organisms such as fungi by interfering with the translocation step in protein synthesis. It inhibits translation elongation through binding to the E-site of the 60S ribosomal unit and interfering with deacetylated tRNA (1-3) |
CELL WALL INHIBITORS
Antibiotics in this category disrupt the cell wall of bacteria (inclusive of Gram positive and Gram negative bacteria). Examples of antibiotics that are cell wall inhibitors include: penicillins, cephalosporins, vancomycin, monobactams and other anti-mycobacterial agents that specifically target the cell wall of mycobacteria (whose cell wall contain mycolic acid). Antibiotics that are cell wall inhibitors are only effective against bacteria with cell wall. They have no activity on bacteria that do not have cell wall (e.g. mycoplasmas). Cell wall inhibitors basically stop the synthesis of peptidoglycan in bacteria, and this ultimately prevents their cell wall (a natural barrier that controls the flow of molecules in- and out- of the cell) from forming.
PROTEIN SYNTHESIS INHIBITORS
Protein synthesis inhibitors interact with the ribosomes of bacteria (especially the 50S and 30S ribosomes); and this interactions prevents translation in the target bacterial cells. Translation is vital for protein synthesis because it is at this stage that the genetic information encoded by the DNA is decoded by the mRNA for the formation of a specific protein molecule. Bacterial ribosomes are usually 30S, 50S and 70S while the ribosomes of eukaryotic cells particularly humans is 80S. Note: The “S” values attached to the 50S ribosomes or ribosomal subunit is generally referred to Svedberg units; and it shows the sedimentation coefficients of ribosomal subunits (e.g. 30S, 50S and 70S) when they are subjected to centrifugal force in an ultracentrifuge. Streptomycin, chloramphenicol, tetracyclines and erythromycins amongst others are typical examples of antibiotics that are protein synthesis inhibitors but each is specific in action in that they target specific ribosomal subunit of the bacterial cell either 50S or 30S ribosomal subunit.
ANTIBIOTICS THAT DAMAGE BACTERIAL CELL MEMBRANE
Some antibiotics target only the cell membranes of bacteria cells. Examples include the polymyxins. The integrity of the cytoplasmic or plasma membrane is vital for the normal functioning of all bacterial cells. Cytoplasmic membranes act as diffusion barriers to some molecules including water, antibiotics and nutrients. But antibiotics that target bacterial cell membranes destabilizes the plasma membrane, and makes it more permeable to harmful substances including antibiotics that destroy the cell.
NUCLEIC ACID INHIBITORS
Nucleic acid inhibitors are group of antibiotics that target the DNA of bacterial cells. Typical examples of nucleic acid inhibitors include rifampicin, ciprofloxacin and a range of other antimicrobial drugs. Nucleic acid inhibitors target the DNA and RNA synthesis of bacterial cells especially by disrupting the activities of key enzymes required for these processes especially DNA gyrase (topoisomerase II and IV) and RNA polymerase. DNA gyrase enzyme and/or topoisomerases are crucial for the synthesis of nucleic acids (particularly DNA) in bacterial cells; and when their natural activity is interfered with, DNA synthesis will be interrupted. Because the activities of the cell is mainly directed by the DNA (which is the actual genetic material), the bacterial cell will die once its ability to synthesize nucleic acid molecules have been disrupted.
ANTI-METABOLITES
Anti-metabolites are antibiotics that inhibit the metabolic pathways of pathogenic bacteria especially as it relates to the biosynthesis of important molecules in the microbes. They are basically sulpha drugs that interfere with the metabolic pathways responsible for synthesizing important growth molecules (e.g. folic acid) in bacterial cells. Trimethoprim, pyrimethamine and sulphamethoxazole are typical examples of antimetabolites. Generally, anti-metabolites compete for essential metabolites, nutrient molecules or growth factors that are considered necessary in bacterial metabolism especially as it relates to their unperturbed development. Antibiotics in this category are chemically synthesized drugs i.e. they are synthetic agents.
References
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Axelsen P. H (2002). Essentials of Antimicrobial Pharmacology. Humana Press, Totowa, NJ.
Balfour H. H (1999). Antiviral drugs. N Engl J Med, 340, 1255–1268.
Bean B (1992). Antiviral therapy: current concepts and practices. Clin Microbiol Rev, 5, 146–182.
Beck R.W (2000). A chronology of microbiology in historical context. Washington, D.C.: ASM Press.
Champoux J.J, Neidhardt F.C, Drew W.L and Plorde J.J (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases. 4th edition. McGraw Hill Companies Inc, USA.
Chemotherapy of microbial diseases. In: Chabner B.A, Brunton L.L, Knollman B.C, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, McGraw-Hill; 2011.
Chung K.T, Stevens Jr., S.E and Ferris D.H (1995). A chronology of events and pioneers of microbiology. SIM News, 45(1):3–13.
Courvalin P, Leclercq R and Rice L.B (2010). Antibiogram. ESKA Publishing, ASM Press, Canada.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Hugo & Russell’s Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA. Pp.152-172.
Dictionary of Microbiology and Molecular Biology, 3rd Edition. Paul Singleton and Diana Sainsbury. 2006, John Wiley & Sons Ltd. Canada.
Drusano G.L (2007). Pharmacokinetics and pharmacodynamics of antimicrobials. Clin Infect Dis, 45(suppl):89–95.
Engleberg N.C, DiRita V and Dermody T.S (2007). Schaechter’s Mechanisms of Microbial Disease. 4th ed. Lippincott Williams & Wilkins, Philadelphia, USA.
Finch R.G, Greenwood D, Norrby R and Whitley R (2002). Antibiotic and chemotherapy, 8th edition. Churchill Livingstone, London and Edinburg.
Ghannoum MA, Rice LB (1999). Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev, 12:501–517.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Gordon Y. J, Romanowski E.G and McDermitt A M (2005). A review of antimicrobial peptides and their therapeutic potential as anti-infective drugs. Current Eye Research, 30(7): 505-515.
Hardman JG, Limbird LE, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 10th ed. New York: McGraw-Hill; 2001.
Joslyn, L. J. (2000). Sterilization by Heat. In S. S. Block (Ed.), Disinfection, Sterilization, and Preservation (5th ed., pp. 695-728). Philadelphia, USA: Lippincott Williams and Wilkins.
Katzung, B. G. (2003). Basic and Clinical Pharmacology (9th ed.). NY, US, Lange.
Kontoyiannis D.P and Lewis R.E (2002). Antifungal drug resistance of pathogenic fungi. Lancet. 359:1135–1144.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.