Opportunistic mycoses are fungal infections caused by opportunistic fungi that only affect people with weakened immune system. They do not occur in healthy people. Opportunistic mycoses are fungal infections of the body which occur almost exclusively in debilitated patients whose normal defense mechanisms against infections are impaired. Such patients include those on chemotherapy, cancer patients, patients who use corticosteroids, organ transplant patients and patients with HIV/AIDS infection.
The fungi that cause opportunistic mycoses are usually fungal organisms that have a very low inherent virulence; and thus lack the natural ability to cause infection in individuals whose immune system is still intact. Only people with poor or compromised immunity are mostly affected by opportunistic fungi.
Opportunistic mycoses include candidiasis, aspergillosis, mucormycosis, systemic penicilliosis and pneumocystis pneumonia (Table 1); and cryptococcosis. It is noteworthy that all opportunistic mycoses are exogenous infections acquired from the environment via the inhalation of viable fungal spores excluding candidiasis which is endogenous because the causative agent (C. albicans) is part of the host’s normal microflora.
Opportunistic microorganisms inclusive of bacteria and fungi are commensal organisms which exist in the environment as free-living and harmless microbes. However, these avirulent organisms become pathogenic and virulent when they come in contact with people with compromised immunity i.e. those with debilitating disease or weakened resistance to infections (e.g. HIV/AIDS patients).
Other predisposing factors to the acquisition of opportunistic mycoses include prolonged antibiotic usage, use of immunosuppressive drugs, chemotherapy, leukaemia and cancer amongst other debilitating diseases. The fungal genera routinely encountered in the microbiology laboratory as causative agents of opportunistic mycoses include Candida, Aspergillus, Mucor, Cryptococcus and Pneumocystis. Other causative agents of opportunistic mycoses include phaeohyphomycetes, hyalohyphomycetes, Penicillium marneffei, Pseudallescheria boydii and Fusarium species amongst other opportunistic yeasts.
Table 1. Synopsis of opportunistic mycoses
| Mycoses | Causative agent | Clinical feature | Site of infection |
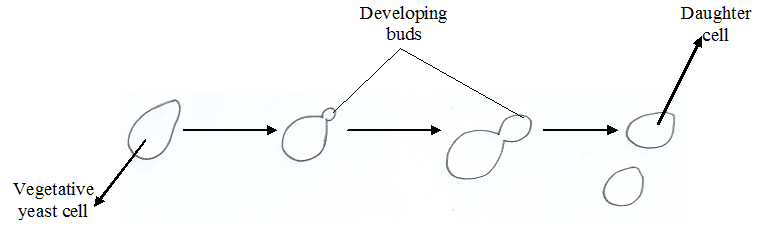
| Candidiasis | C. albicans. Found as normal flora in the vagina, gut, respiratory tract and mouth | Candidiasis is an endogenous opportunistic infection that affects the mucosal regions of the body (e.g. mouth, gut and vagina) to produce different localized infections such as thrush in the mouth and vulvovaginitis characterized by itching and mucopurulent discharge in the vagina. Systemic disease occurs when the yeasts become disseminated via bloodstream to other vital organs (e.g. heart and kidney). The various clinical forms of candidiasis include vaginal candidiasis, oral candidiasis, cutaneous candidiasis, mucosal & mucocutaneous candidiasis & systemic candidiasis. | Mouth, gut, skin and vagina |
| Aspergillosis | Aspergillus species (e.g. A. Fumigatus and A. flavus) | Aspergillosis is a chronic and acute pulmonary disease usually characterized by the production of aspergilloma (fungus ball) in the lung cavities. It is a tuberculosis-type of pneumonia caused by a fungus in humans. The different clinical forms of aspergillosis include pulmonary aspergillosis, invasive aspergillosis, allergic aspergillosis and extra-pulmonary aspergillosis. | Lungs, skin and other organs in disseminated or invasive aspergillosis |
| Mucormycosis (zygomycosis) | Rhizopus species, Mucor species, Absidia species and Rhizomucor species | Mucormycosis is a pulmonary and paranasal disease that proliferates in the walls of blood vessels especially those of the nasal cavity, lungs and gut. The different clinical forms of zygomycosis include pulmonary, cutaneous, gastrointestinal, rhinocerebral & disseminated mucormycosis. There is usually thrombosis, infarction & necrosis at the sites of infection especially the sinuses, eye and brain. Generally, agents of mucormycosis have high affinity for vascular issues. | Lungs |
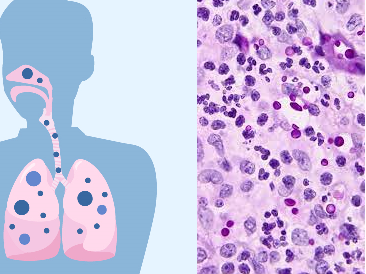
| Pneumocystis pneumonia (pneumocystosis) | Pneumocystis carinii, a yeast previously classified as a protozoan | Pneumocystosis is an interstitial pneumonia that occurs in immunocompromised hosts following depletion of the cell-mediated immunity. The alveolar epithelium or alveoli of the lungs is mostly affected. Extra-pulmonary infections involve the CNS, spleen, eye, middle ear and the liver. Symptoms may include nonproductive cough, fever, dyspnea, malaise & shortness of breath. | Lungs and other associated organs |
| Systemic penicilliosis | Penicillium marneffei | Systemic penicilliosis is a tuberculosis-like pneumonia disease in immunocompromised persons. Symptoms include anaemia, weight loss, skin lesions and fever. The disease is widespread in Asia; and the causative agent is reserved in rodents (e.g. bamboo rats). | Skin and lungs |
References
Anaissie E.J, McGinnis M.R, Pfaller M.A (2009). Clinical Mycology. 2nd ed. Philadelphia, PA: Churchill Livingstone Elsevier. London.
Beck R.W (2000). A chronology of microbiology in historical context. Washington, D.C.: ASM Press.
Black, J.G. (2008). Microbiology: Principles and Explorations (7th ed.). Hoboken, NJ: J. Wiley & Sons.
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA.
Brown G.D and Netea M.G (2007). Immunology of Fungal Infections. Springer Publishers, Netherlands.
Calderone R.A and Cihlar R.L (eds). Fungal Pathogenesis: Principles and Clinical Applications. New York: Marcel Dekker; 2002.
Chakrabarti A and Slavin M.A (2011). Endemic fungal infection in the Asia-Pacific region. Med Mycol, 9:337-344.
Champoux J.J, Neidhardt F.C, Drew W.L and Plorde J.J (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases. 4th edition. McGraw Hill Companies Inc, USA.
Chemotherapy of microbial diseases. In: Chabner B.A, Brunton L.L, Knollman B.C, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, McGraw-Hill; 2011.
Chung K.T, Stevens Jr., S.E and Ferris D.H (1995). A chronology of events and pioneers of microbiology. SIM News, 45(1):3–13.
Germain G. St. and Summerbell R (2010). Identifying Fungi. Second edition. Star Pub Co.
Ghannoum MA, Rice LB (1999). Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev, 12:501–517.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Larone D.H (2011). Medically Important Fungi: A Guide to Identification. Fifth edition. American Society of Microbiology Press, USA.
Levinson W (2010). Review of Medical Microbiology and Immunology. Twelfth edition. The McGraw-Hill Companies, USA.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of Microorganisms, 12th edition. Pearson Benjamin Cummings Inc, USA.
Mahon C. R, Lehman D.C and Manuselis G (2011). Textbook of Diagnostic Microbiology. Fourth edition. Saunders Publishers, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.