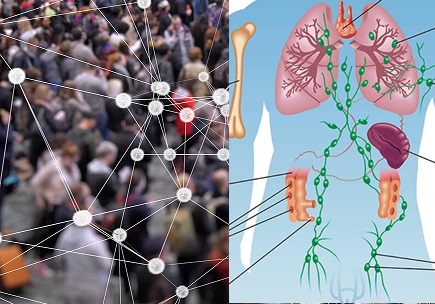
Herd immunity is a group resistance of a population against a particular disease and the spread of its disease-causing agent in the same population. It is a collective type of immunity that is demonstrated by a community against a particular pathogen and disease within the same environment. In herd immunity, there are a larger proportion of individuals who are protected against an infection in a population, and this allows members of the community to enjoy an immunity which is not necessary of their own making but that of the community they found themselves.
This type of immunity reduces the probability of effective contacts of infective persons with those that are vulnerable while allowing susceptible individuals in the community to have contacts with those that are already immune against a given infection. Herd immunity allows epidemiologists the chance of assessing epidemic developments within a population. A higher proportion of immune individuals within a given community will ensure a higher proportion of protected population.
This is the rationale behind most public immunization programs (e.g. polio immunization). When immunization exercises are embarked upon and routinely followed, the goal is to ensure that herd immunity is maintained in the population by reducing the number of susceptible individuals which continue to enter the population via many means such as child birth and migration.
Antigenic shift and antigenic drift of pathogenic microorganisms can also inform the decision of public health professionals and health policy makers to step up their immunization programs and monitoring and evaluation of the exercise in a given population.
It is however noteworthy that herd immunity (which can also be called community immunity or population immunity) does not necessarily work for those infectious diseases that have a common source of transmission or spread in a given population. Cholera (caused by Vibrio cholerae) is a typical example of an infection or disease that has a common source of transmission.
The common source of cholera transmission or spread in a population is contaminated water especially those contaminated with human excreta or sewage. Individuals who drink form such feacally-contaminated water will easily become infected with V. cholerae and other infectious disease agents transmitted through this route; and this will predispose those affected to a variety of waterborne diseases (despite the fact that the hosts are immune or non-immune).
Microbial diseases that come from a common source (e.g. water and food) is transmitted in a given population via that common source – irrespective of the fact that some individuals in the said community or population may be immune or non-immune, susceptible or non-susceptible hosts.
Since the members of the community (inclusive of the immunized and non-immunized members) drink or get their water from the same contaminated common source, they all can easily become infected or acquire the disease agent once the source of their water is contaminated by microbial pathogens.
Herd immunity as aforementioned is the indirect form of protection that occurs when a large proportion of a population have become immune to an infectious disease such as measles or polio – thereby providing a reasonable form of immunity for non-immunized members of the same community that they come in direct contact with.
It can be achieved through massive immunization or vaccination of a large percentage of the population; and this epidemiological concept (i.e. herd immunity is vital to halting disease transmission or spread in any given population, especially those infectious diseases transmitted or acquired via direct body contact with infected individuals – which are the types of diseases preventable via the phenomenon of herd immunity.
Infectious diseases that can be transmitted via direct body contact with infected persons are typical examples of diseases that are preventable via herd immunity – in which a larger proportion of the population are immunized, thus body contacts in the population is now with immunized individuals (who do not spread the disease) rather than with non-immunized and possibly chronic carriers (who will definitely spread the disease in the population).
References
Aschengrau A and Seage G.R (2013). Essentials of Epidemiology in Public Health. Third edition. Jones and Bartleh Learning,
Aschengrau, A., & G. R. Seage III. (2009). Essentials of Epidemiology in Public Health. Boston: Jones and Bartlett Publishers.
Bonita R., Beaglehole R., Kjellström T (2006). Basic epidemiology. 2nd edition. World Health Organization. Pp. 1-226.
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA.
Castillo-Salgado C (2010). Trends and directions of global public health surveillance. Epidemiol Rev, 32:93–109.
Centers for Disease Control and National Institutes of Health (1999). Biosafety in Microbiological and Biomedical Laboratories, 4th edn, Washington DC: CDC.
Gordis L (2013). Epidemiology. Fifth edition. Saunders Publishers, USA.
Guillemin J (2006). Scientists and the history of biological weapons. European Molecular Biology Organization (EMBO) Reports, Vol 7, Special Issue: S45-S49.
Halliday JE, Meredith AL, Knobel DL, Shaw DJ, Bronsvoort BMC, Cleaveland S (2007). A framework for evaluating animals as sentinels for infectious disease surveillance. J R Soc Interface, 4:973–984.
Lucas A.O and Gilles H.M (2003). Short Textbook of Public Health Medicine for the tropics. Fourth edition. Hodder Arnold Publication, UK.
MacMahon B., Trichopoulos D (1996). Epidemiology Principles and Methods. 2nd ed. Boston, MA: Little, Brown and Company. USA.
Nelson K.E and Williams C (2013). Infectious Disease Epidemiology: Theory and Practice. Third edition. Jones and Bartleh Learning.
Porta M (2008). A dictionary of epidemiology. 5th edition. New York: Oxford University Press.
Rothman K.J and Greenland S (1998). Modern epidemiology, 2nd edition. Philadelphia: Lippincott-Raven.
Rothman K.J, Greenland S and Lash T.L (2011). Modern Epidemiology. Third edition. Lippincott Williams and Wilkins, Philadelphia, PA, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.