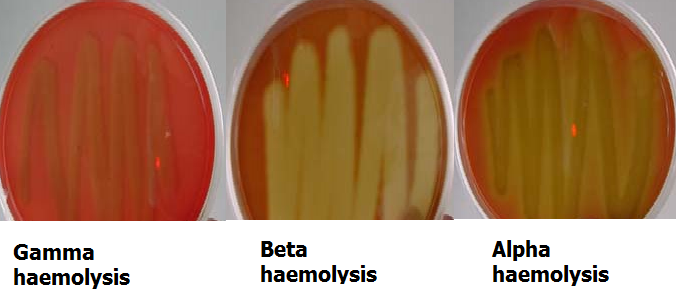
Streptococcus pyogenes is a Group A Streptococcus species that is non-spore forming, Gram-positive, non-motile round to ovoid bacterium that occur in chains, singly (as coccus) or in pairs (as diplococci). It is the most common cause of pharyngitis (sore throat) in humans. Other streptococcal diseases caused by Streptococcus species in humans include scarlet fever, cellulitis, necrotizing fasciitis, erysipelas, impetigo, tonsillitis, pneumonia, otitis media, and septicaemia. S. pyogenes is a beta-haemolytic Streptococcus species that is catalase negative and facultatively anaerobic. It requires enriched media (e.g. agar supplemented with sheep blood) to grow effectively in the laboratory.
Streptococcus species are complex bacterial species classified into different groups based on their clinical significance and ability to haemolyse or breakdown blood. Some of the notable Streptococcus groups are Group A streptococci (e.g. S. pyogenes) which cause beta-haemolysis, Group B streptococci (e.g. S. agalactiae) which cause α, β, and γ haemolysis, Viridans streptococci group (which contain non-typable or groupable Streptococci species such as S. mutans), Group D streptococci (e.g. Enterococcus faecalis and S. bovis), and other untypable or ungroupable Streptococcus species including S. pneumoniae (pneumococcus) that has no specific antigenic substance for their grouping.
The groupings of Streptococcus species is based on serological data and/or specific antigenic structures associated with each of the streptococcal species, and this classification is based on the Lancefield classification – which classifies bacteria according to specific cell wall and capsular antigens found on the bacteria. E. faecalis is also known as S. faecalis. Lancefield classification (as described by the famous microbiologist Rebecca Lancefield) grouped Streptococcus species into groups A-O. Rebecca Lancefield successfully demonstrated the presence of specific carbohydrate antigens in the cell wall extracts of beta-haemolytic Streptococcus species, and it is upon this basis that most streptococcal species are classified.
Lancefield established the definitive identification of Streptococcus species based on the serologic reactivity of cell wall polysaccharide antigens of the bacteria. The Viridans streptococci are streptococcal species that do not contain any of the Lancefield grouping antigens; and these streptococcal species are often found in the upper respiratory tract of humans and other animals. Other Viridans streptococci are S. sanguis, S. oralis and S. salivarius. S. pyogenes is a member of the human normal microflora, and they are widespread in nature.
Many healthy people are asymptomatic carriers of S. pyogenes. Pus-forming infections and upper respiratory infections usually occur in humans when the body’s immune system is weakened; and the mode of transmission of the pathogen is via direct or indirect contacts with respiratory droplets of infected persons. The throat and skin are the main reservoir of S. pyogenes in the human body.
PATHOGENESIS OF STREPTOCOCCUS PYOGENES INFECTION
S. pyogenes causes infections of the upper respiratory tract and other invasive infections of the skin and connective tissues of humans. Like Staphylococcus species, S. pyogenes produces a wide variety of virulence factors which spur the many diseases that they produce in humans. Some of the extracellular enzymes and toxins produced by S. pyogenes include streptolysin O and S, streptokinase, Dnase, hyaluronidase, M protein, haemolysins, and streptococcal pyrogenic exotoxins. Streptolysin O (SO) is an immunogenic, haemolytic and cytolytic toxin produced by S. pyogenes. It is antigenic in nature, thus stimulating the production of anti-streptolysin O (ASO) antibody in infected individuals; and can be used to diagnose recent S. pyogenes infections.
SO is oxygen-labile (i.e. it is not active in the presence of oxygen), and is thus inactivated by oxidation. Streptolysin S (SS) is a non-immunogenic, haemolytic, oxygen-stable toxin produced by S. pyogenes. SS is not antigenic, and thus forms no antibody in infected individuals. Both SO and SS destroy the cell membranes of red blood cells (RBCs) and other host cell membranes. Streptococcal pyrogenic exotoxins also known as erythrogenic toxin is mainly responsible for the rashes produced in scarlet fever infection; and the toxins (which are superantigens) produces similar clinical signs as that of toxic shock syndrome toxin (TSST) caused by S. aureus.
M protein (fibronectin-binding protein) appears as hair-like structures on the cell wall of S. pyogenes; and it is primarily responsible for protecting the pathogen from host phagocytic action. S. pyogenes gains entry into the human body through mucous membranes or fractured skin; and the pathogen multiplies rapidly and evades some mechanisms of the host immune system (e.g. phagocytosis).
Upon entry, the pathogen causes a variety of acute, invasive and systemic infections such as impetigo (infection of the superficial layers of the skin), scarlet fever, a widespread skin rash (Figure 1), rheumatic fever (autoimmune disease involving the joints), necrotizing fasciitis (inflammation of skeletal muscles), pharyngitis (sore throat infection), tonsillitis (inflammation of the tonsils), cellulitis (infection of the deep layers of the skin), puerperal fever (sepsis after childbirth) and other severe invasive infections that may affect the heart and kidney and other vital organs of the body.

LABORATORY DIAGNOSIS OF STREPTOCOCCUS PYOGENES INFECTION
The laboratory diagnosis of S. pyogenes infections is based on the isolation and identification of the pathogen in culture and through microscopic and serological tests. Throat swab, wound swab, blood, pus and swabs from skin lesions are some clinically important specimens required for the laboratory diagnosis of S. pyogenes infections. Latex agglutination tests that detect ASO produced by S. pyogenes are commercially available for laboratory diagnosis of the disease.
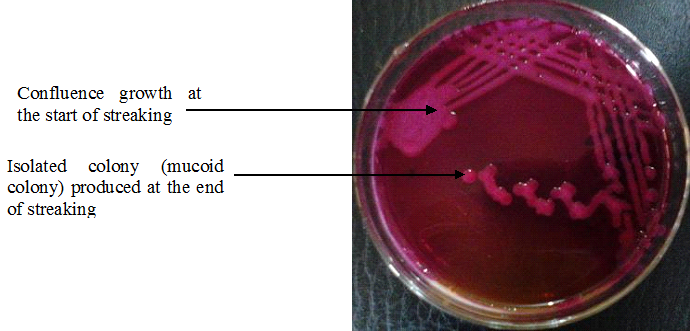
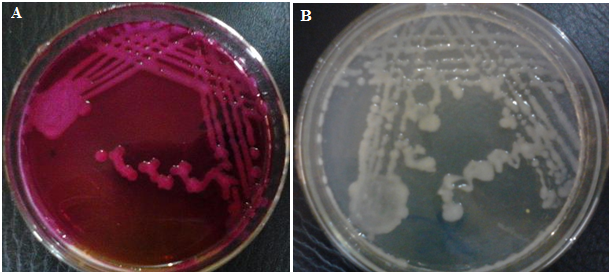
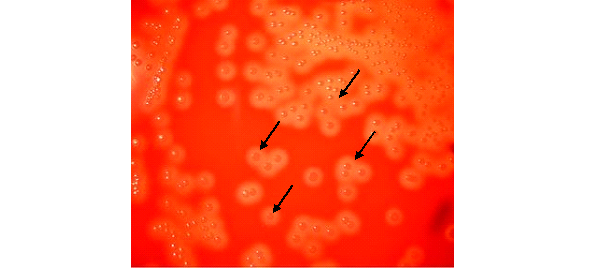
Gram stained smears of wound infections and skin lesions may prove diagnostic but stained smears of samples in pharyngitis are clinically irrelevant because Viridans Streptococci species are members of the human normal floraand may be indistinguishable from S. pyogenes in stained smears. Rapid diagnostic test kits (e.g. ELISA) are usually employed in the laboratory diagnosis of sore throat caused by S. pyogenes. S. pyogenes grow on blood agar and chocolate agar to produce small haemolytic colonies (Figure 2). S. pyogenes is susceptible to bacitracin but not optochin; and biochemically, it is catalase negative.
IMMUNITY TO STREPTOCOCCUS PYOGENES INFECTION
Coughing and sneezing are some nonspecific immune mechanisms used to prevent S. pyogenes from penetrating beyond the superficial epithelium of the upper respiratory tract while the activities of the phagocytes act as a second line of defense against invading Streptococcus species. The production of ASO in infected individuals does not indicate any future protection from the pathogen. Some recurring infections due to S. pyogenes can occur in infected individuals if infection is caused by a different strain. Immunity against most streptococcal disease is type-specific i.e. resistance is only developed against a specific type of invading pathogen. New strains can cause infection because the host body lacks immunity against it.
TREATMENT OF STREPTOCOCCUS PYOGENES INFECTION
Therapy for S. pyogenes infections is based on antimicrobial susceptibility test result and the type of prevailing disease. Penicillin G, erythromycin, cephalosporins and fluoroquinolones are some of the antibiotics of choice used to manage infections caused by S. pyogenes. Treatment of Streptococcal infections is important in order to prevent the spread of the pathogen to susceptible individuals and also to ease the already infected patient from the symptoms of the disease.
PREVENTION AND CONTROL OF STREPTOCOCCUS PYOGENES INFECTION
No vaccine currently exists for immunization against diseases caused by S. pyogenes. Vaccines are only available for infections caused by S. pneumoniae. Prevention and control of S. pyogenes infection transmission is usually based on effective treatment of infected individuals. Prophylactic and chemoprophylactic measures can also be used for susceptible individuals and those who may have suffered from some forms of the disease (e.g. rheumatic fever). The transmission of S. pyogenes infections (especially those that affect the upper respiratory tract) is through direct or indirect contact with respiratory fluids from infected persons. Thus, infected individuals should be properly treated, and contact with non-infected people should be restricted as much as possible.
OTHER SPECIES OF STREPTOCOCCUS
- Streptococcus pneumoniae: S. pneumoniae (pneumococcus) is a normal inhabitant of the human upper respiratory tract; and the bacterium mainly causes pneumonia otherwise known as pneumococcal pneumonia [Pneumonia is a disease of the lung that is caused by different bacteria including Streptococcus, Staphylococcus, Pseudomonas, Haemophilus, Chlamydia and Mycoplasma, several viruses, and certain fungi and protozoa] in humans. Pneumococcus (S. pneumoniae) is also implicated in a variety of other bacterial-related diseases including osteomyelitis, septic arthritis, endocarditis, peritonitis, paranasal sinusitis, otitis media, meningitis, cellulitis and brain abscesses. S. pneumoniae is currently the leading cause of invasive bacterial disease in children and the elderly.
- S. agalactiae: S. agalactiae is a beta-hemolytic, catalase-negative, and facultative anaerobe of the genus Streptococcus. It is a harmless commensal bacterium that colonizes the gastrointestinal and genitourinary tract of humans especially adults as normal microflora. S. agalactiae can also be called group B streptococcus (GBS). GBS is the major cause of several bacterial-related infections of the newborn; and it is also implicated in cases of septicemia, pneumonia, and meningitis. It is the most common pathogen causing neonatal infection in neonates; and neonatal infection often results from Streptococcus contamination of the lower reproductive tract of infected mothers during child birth. GBS infection in adults includes urinary tract infections (UTIs), skin and soft-tissue infection, bacteremia, osteomyelitis, meningitis and endocarditis.
- S. canis: S. canis is a group G beta-hemolytic species of the genus Streptococcus. It was first isolated in dogs. S. canis is an important normal microflora in cats and dogs; and human infection with the organism is rare. However, S. canis is can cause bovine mastitis in cows.
- S. bovis: S. bovis is a known human pathogen that has been implicated as a causative agent of endocarditis, UTIs, and more rarely, septicemia and neonatal meningitis. However, the organism is commonly found in the alimentary tract of cattle, sheep, and other ruminants (four-chambered stomach animals) – where they cause a condition known as ruminal acidosis or feedlot bloat. S. bovis is a lactic acid bacterium (i.e. it has the ability to ferment or breakdown carbohydrates to lactic acid molecules). Ruminal acidosis (feedlot bloat) occurs in ruminants when they consume starch diets. Diets high in starch or sugar (i.e. fermentable carbohydrates) promote the proliferation of S. bovis in the rumen of ruminants. As a lactic acid bacterium, S. bovis ferments the carbohydrates in the ruminant’s rumen to lactic acid. This causes a decline in the pH of the rumen – which leads to the development of adverse conditions such as ruminal acidosis or feedlot bloat.
- S. mitis: S. mitis is a commensal bacterium that colonizes hard surfaces in the oral cavity of humans such as the dental hard tissues and mucous membranes. It is most commonly found in the throat, nasopharynx, and mouth as normal microflora. S. mitis is usually an etiologic agent in odontogenic infections and endocarditis in humans.
- S. mutans: S. mutans is commonly found in the human oral cavity as a normal microflora, and it is a common cause of tooth decay in humans. It significantly contributes to oral disease of man. S. mutans is the primary causal agent and the pathogenic species responsible for dental caries (tooth decay or cavities); and its ability to do this is due to its cariogenic potential. S. mutans has a natural ability to metabolize various sugars and produce acids and other substances or compounds such as biofilms which destroy the teeth.
- S. sanguinis: S. sanguinis was formerly known as S. sanguis. It is found in the human oral cavity as a normal microflora. It can cause bacterial endocarditis when it becomes systemic or enters the bloodstream through dental surgery. S. sanguinis is found in dental plaque.
- S. intermedius: S. intermedius is usually isolated from the anterior nares of pigeons, dogs, mink, and horses.
- S. anginosus: S. anginosus is part of the human bacteria flora found in various part of the body including the mouth, sinuses, throat, and vagina. It can cause diseases including brain and liver abscesses and bacteraemia.
- S. salivarius: S. salivarius is an opportunistic species of the genus Streptococcus that colonizes the mouth and upper respiratory tract of healthy humans few hours after birth.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.