The phrase sterility simply means the absence of living organisms including bacteria, fungi, viruses, protozoa and other vegetative cells in a product. Sterility is usually achieved through the process of sterilization. And sterilization is defined as the process of by which objects, materials or environments can be rendered sterile (i.e. free from living organisms). Sterilization can be achieved by several methods including autoclaving, filtration, heating, use of ethylene oxide gas and by ionizing radiation. Microbiological and/or biochemical tests carried out on biological products are necessary in order to ensure that the products are not just efficacious but also safe for human and/or animal consumption.
The term sterility is usually an absolute term – which implies the complete absence of viable microorganisms in a product or in an environment. But in practice, the sterility of a product is defined by the absence of viable and actively multiplying microorganisms when tested in specified culture (nutrient) media that supports the growth of the microbes. Usually, culture (nutrient) media that support the growth of suspected contaminants including bacteria and fungi are used for the isolation of microbes from the tested samples that representative of the batch of product to be tested.
Sterility tests are microbiological and/or biochemical tests carried out on biological products, food and other pharmaceutical products in order to critically assess their freedom from contaminating microorganisms including mycoplasma, bacteria, fungi and viruses. Such tests are usually intended to detect the possible presence of viable microorganisms in a given biological or pharmaceutical products. Several products ranging from medicines, food and vaccines are subjected to series of sterility tests that ascertain their freedom from contamination or pathogenic microbes. Sterility tests are critical in the production of biological products since they are intended for parenteral (systemic) administration – and in which case they either confer health benefits or therapeutic effects on the consumers.
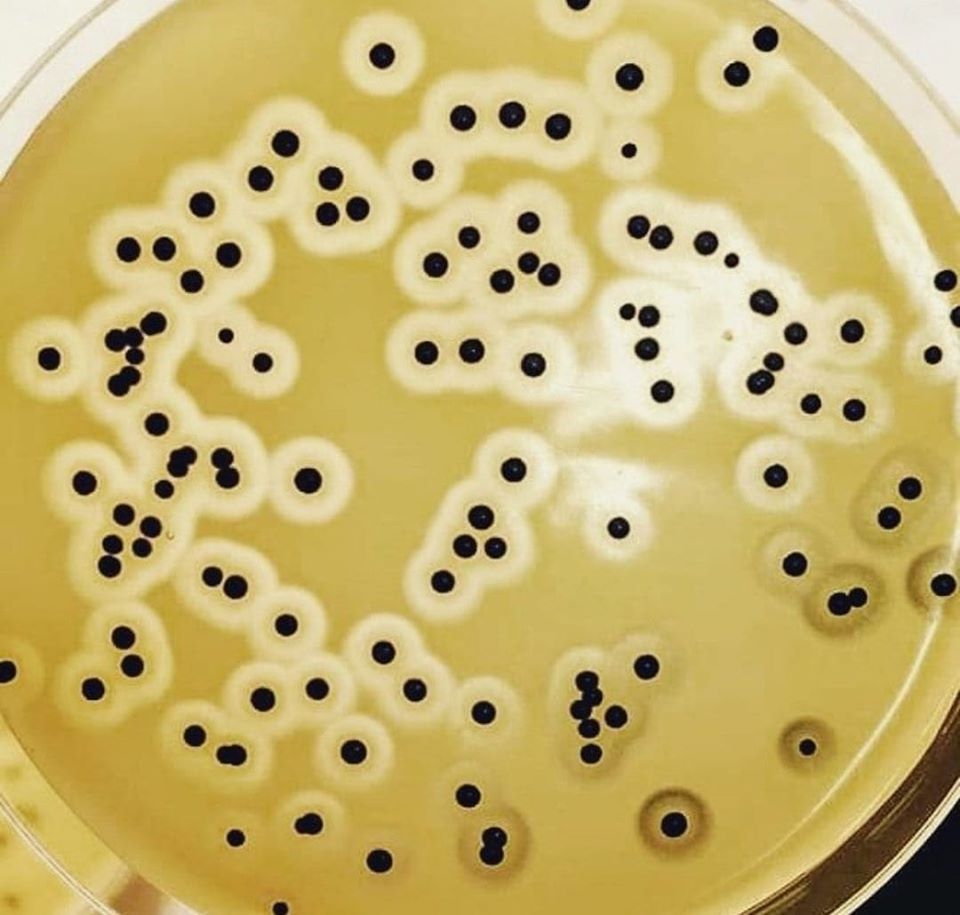
Because sterility is an absolute term, it is vital to ensure that the working environments in which sterility tests are carried out in are free from contaminating microbes; and it is also important to avoid any accidental contamination of the product being tested. The principle supporting the sterility tests of biological products is simply based on the fact that microorganisms are ubiquitous and thus could find their way into products during production. And if this is the case, when such contaminated product is subjected to sterility tests using appropriate culture media, it is expected that the contaminating organisms will grow and produce colonies (in the case of solid culture media plates) or turbidity and/or gas production (for broth cultures) that gives impetus to the presence of contaminating microorganisms. Sterility tests are adequately designed in such a manner that they reveal the presence of contaminating microorganisms present in the test samples used for the experiment. It is noteworthy that sterility test is not performed on all the products but on some representative samples of the whole lot or batch – since it is not practicably possible to test all the samples or products in a batch of product.
Nevertheless, a sufficient number of product samples from each batch of the product are subjected to sterility testing in order to give “an acceptable degree of confidence” in the ultimate results obtained from the sterility test; and thus certify the batch of the product free from contaminating microorganisms. A sampling technique based on probability profile is used to select samples from a batch of product for sterility testing since not all the samples or products in a batch can be tested at the same time.
Sampling is defined as the statistical process of selecting a part or portion of a whole product batch to represent the entire batch. And samples are picked or selected in a random manner to serve as representative samples of the whole lot. The use of membrane filtration technique and direct inoculation using culture (nutrient) media are often the two most important principal sterility testing technique used to determine the sterility of a product. Membrane filtration technique is indispensable in sterility testing because of the assumption that microorganisms especially bacteria will not pass through a membrane filter of 45 mm (0.45 µm) porosity. However, there also exist some rapid techniques employed for the determination of the sterility of a product.
Some of these rapid techniques include the ATP-bioluminescence, colorimetric growth detection technique, autofluorescence and the use of cytometry. Sterility tests only detect gross contamination of those microorganisms which will produce visible turbidity in broth culture media (as evidence of microbial growth) or produce gas or acid as a result of microbial activity. Factors that affect the sterility tests include number of samples used, and testing conditions such as media used and incubation conditions for growth. The sterility test will only detect or show the presence of those microorganisms that will grow under the provided test conditions even when testing products suspected of heavy microbial contamination. These test conditions include the type of culture media used, incubation temperature, diluents used and recovery methods.
Generally, sterility testing is a regulatory requirement for the release of biological and pharmaceutical products that cannot be terminally sterilized (i.e. products that are heat-labile and thus susceptible to destruction by heat); and sterility test still remain a pass for the release of biological products for public consumption. Since sterility testing cannot on its own certify the absolute assurance of freedom of a product from microbial contamination, it is vital that every manufacturing processes (especially those meant for the production of biological products) ensures a continued and strict compliance to Good Manufacturing Practices (GMPs) at every production stage. This implies that the possible microbial contamination of the process and/or product should be prevented before it happens. Thus, the quality systems of production and/or manufacturing units should ensure aseptic process, proper sterilization techniques, sterility assurance, quality control and assurance; and the microbiological and physical parameters of the production process should be continuously monitored during production to minimize contamination of the finished biological products.
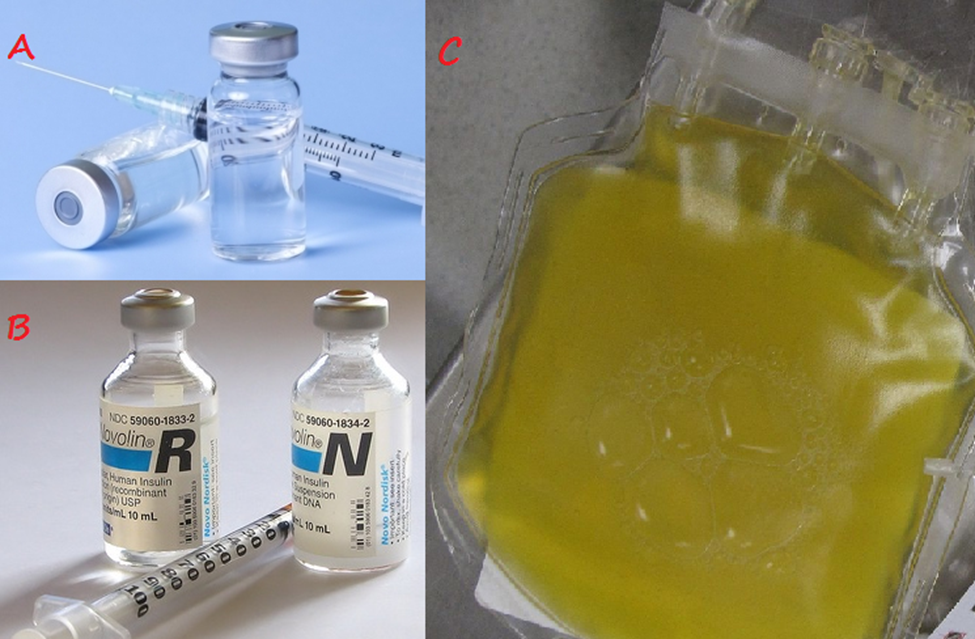
Biological products are medical products intended for the prevention, treatment or cure of a disease condition in humans or animals; and they are also used to prevent or diagnose diseases. Many biological products are made from a variety of natural sources that includes humans, animals, plants and microorganisms. Typical examples of biological products include: vaccines, human insulin, monoclonal antibodies, blood and blood products for transfusion and/or manufacturing into other products, allergenic extracts (which are used for both diagnosis and treatment of allergic conditions), human cells and tissues used for transplantation, gene therapy products, cellular therapy products and test kits to screen potential blood donors for infectious agents such as human immunodeficiency virus (HIV) (Figure 1).
Biological products or biologics can be composed of sugars, proteins, or nucleic acids, or a combination of these substances; and they may also be living entities, such as cells and tissues. Biological products are produced by biotechnology methods in commercial quantities. Biological products can also be known as biopharmaceuticals. Biological products or biologics differ from the conventional drugs in several ways. In contrast to most drugs that are chemically synthesized and with known structures, most biological products are complex mixtures that are not easily identified or characterized. Biological products are usually heat sensitive and thus susceptible to microbial contamination.
This is why it is important to always ensure aseptic techniques in the production of these biologics from the initial stage of manufacturing to the last stage of manufacturing. Contamination of biological products during production could result from the personnel involved in the production process; equipments and instruments used for the production; raw materials including water used for the production; and the production environment or facility. The production environment and/or facility involved for the production of biological products should be as sterile as possible (i.e. free from all viable microorganisms capable of causing contamination) in other to ensure that the biological products are fit for animal or human consumption.
Materials used in the production of biological products should be sterilized and/or tested in order to ensure that they are free from contaminants including microbes before being used or released for public consumption. Samples of the finished biological product should also be tested for the presence of bacterial, fungal, or mycoplasmal contaminants. The primary raw materials for biological production should be collected from sources shown to be free from contamination and they should be handled in such a way as to minimize contamination and the opportunities for any form of microbial contaminant to multiply in them.
The materials should be properly sterilized using suitable sterilization techniques that will not affect the quality, texture and the biological activity inherent in them. Raw materials that are not sterilized and those that are to be processed further after sterilization should be handled aseptically to avoid possible contamination either during storage or handling. And the environments in which these materials are processed should always be maintained in a clean state and protected from external sources of microbial contamination. Internal contamination of the clean rooms should also be avoided as much as possible by ensuring aseptic technique at each stage of the production.
References
Arora D.R (2004). Quality assurance in microbiology. Indian J Med Microbiol, 22:81-86.
Ashutosh Kar (2008). Pharmaceutical Microbiology, 1st edition. New Age International Publishers: New Delhi, India.
Axelsen P.H (2002). Essentials of antimicrobial pharmacology. Humana Press, Totowa, New Jersey, USA. Al-Jasser A.M (2006). Extended – Spectrum Beta – Lactamases (ESBLs): A Global Problem. Kuwait Medical Journal, 38(3):171-185.
Bisht R., Katiyar A., Singh R and Mittal P (2009). Antibiotic Resistance – A Global Issue of Concern. Asian Journal of Pharmaceutical and Clinical Research, 2 (2):34-39.
Block S.S (2001). Disinfection, sterilization and preservation. 5th edition. Lippincott Williams & Wilkins, Philadelphia and London.
Cars O and Nordberg P (2005). Antibiotic resistance: The faceless threat. International Journal of Risk & Safety in Medicine, 17 (3/4): 103-110.
Carson C.F., Hammer K.A and Riley T.V (2006). Malaleuca alternifolia (Tea Tree) oil: A Review of Antimicrobial and other Medicinal Properties. Clinical Microbiology Review, 19(1):50-62.
Cowan M.M (1999). Plant products as antimicrobial agents. Clinical Microbiology Reviews., 564-582.
Denyer S.P., Hodges N.A and Gorman S.P (2004). Pharmaceutical Microbiology. 7th ed. Blackwell Publishing Company, USA.
Ejikeugwu Chika, Ikegbunam Moses, Ugwu Chigozie, Eze Peter, Iroha Ifeanyichukwu, and Esimone Charles (2013). Phenotypic Detection of Klebsiella pneumoniae Strains – Producing Extended Spectrum β-Lactamase (ESBL) Enzymes. Scholars Academic Journal of Biosciences. 1(1):20-23.
Ejikeugwu Chika, Iroha Ifeanyichukwu, Adikwu Michael and Esimone Charles (2013). Susceptibility and Detection of Extended Spectrum β-Lactamase Enzymes from Otitis Media Pathogens. American Journal of Infectious Diseases. 9(1):24-29.
Ejikeugwu Chika, Iroha Ifeanyichukwu, Adikwu Michael and Esimone Charles (2013). Susceptibility and Detection of Extended Spectrum β-Lactamase Enzymes from Otitis Media Pathogens. American Journal of Infectious Diseases. 9(1):24-29.
Ejikeugwu Chika, Ugwu C.M., Ikegbunam N.M, Araka C.O., Iroha I.R., Adikwu M.U and Esimone C.O (2012). Evaluation of antibacterial activity of the leave extracts of Buchholzia coriacea. Asian Journal of Pharmaceutical and Biological Research. 2(4):204-208.
Ejikeugwu Chika, Ugwu Malachy, Iroha Ifeanyichukwu, Gugu Thaddeus, Duru Carissa, Eze Peter, and Esimone Charles (2013). Detection and antimicrobial susceptibility of some Gram negative bacteria producing carbapenemases and extended spectrum beta lactamases. International Journal of Microbiology and Immunology Research, 2(6):064-069.
Ejikeugwu Chika, Umeokoli Blessing, Iroha Ifeanyichukwu, Ugwu Malachy, Esimone Charles (2015). Phytochemical and Antibacterial Screening of Crude Extracts from Leaves of Wonderful Kola. American Journal of Life Sciences. Special Issue: Microbiology Research, 3(2):5-8.
Ejikeugwu P.C., Ugwu C.M., Araka C.O., Gugu T.H., Iroha I.R., Adikwu M.U and Esimone C.O (2012). Imipenem and Meropenem resistance amongst ESBL producing Escherichia coli and Klebsiella pneumoniae clinical isolates. International Research Journal of Microbiology. 3(10):339-344.
Finch R.G, Greenwood D, Norrby R and Whitley R (2002). Antibiotic and chemotherapy, 8th edition. Churchill Livingstone, London and Edinburg.
Joslyn, L. J. (2000). Sterilization by Heat. In S. S. Block (Ed.), Disinfection, Sterilization, and Preservation (5th ed., pp. 695-728). Philadelphia, USA: Lippincott Williams and Wilkins.
Lai P.K and Roy J (2004). Antimicrobial and chemopreventive properties of herbs and spices. Curr. Med. Chem, 11 (11): 1451–1460.
Livermore D.M (2004). The need for new antibiotics. Clinical Microbiology & Infection, 4(10): 1-9.
Mascaretti O.A (2003). Bacteria versus antibacterial agents: An integrated approach. Washington: ASM Press.
Nally J.D (Ed.) (2007). Good manufacturing practices for pharmaceuticals. Sixth edition. Informa Healthcare USA, Inc, New York.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.