Middle East Respiratory Syndrome (MERS) is an illness caused by a virus (more specifically, a coronavirus) called Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Most MERS patients developed severe respiratory illness with symptoms of fever, cough and shortness of breath. About 3 or 4 out of every 10 patients reported with MERS have died.
All cases are linked to the Arabian Peninsula
Health officials first reported the disease in Saudi Arabia in September 2012. Through retrospective (backward-looking) investigations, they later identified that the first known cases of MERS occurred in Jordan in April 2012. So far, all cases of MERS have been linked through travel to, or residence in, countries in and near the Arabian Peninsula. The largest known outbreak of MERS outside the Arabian Peninsula occurred in the Republic of Korea in 2015. The outbreak was associated with a traveler returning from the Arabian Peninsula.
People with MERS can spread it to others
MERS-CoV has spread from ill people to others through close contact, such as caring for or living with an infected person.
MERS can affect anyone. MERS patients have ranged in age from younger than 1 to 99 years old.
SYMPTOMS & COMPLICATIONS
Most people confirmed to have MERS-CoV infection have had severe respiratory illness with symptoms of:
- Fever
- Cough
- Shortness of breath
Some people also had diarrhea and nausea/vomiting. For many people with MERS, more severe complications followed, such as pneumonia and kidney failure. About 3 or 4 out of every 10 people reported with MERS have died. Most of the people who died had a pre-existing medical condition that weakened their immune system, or an underlying medical condition that hadn’t yet been discovered. Medical conditions sometimes weaken people’s immune systems and make them more likely to get sick or have severe illness.
Pre-existing conditions among people who got MERS have included
- Diabetes
- Cancer
- chronic lung disease
- Chronic heart disease
- Chronic kidney disease
Some infected people had mild symptoms (such as cold-like symptoms) or no symptoms at all.
The symptoms of MERS start to appear about 5 or 6 days after a person is exposed, but can range from 2 to 14 days.
TRANSMISSION
MERS-CoV, like other coronaviruses, likely spreads from an infected person’s respiratory secretions, such as through coughing. However, we don’t fully understand the precise ways that it spreads.
MERS-CoV has spread from ill people to others through close contact, such as caring for or living with an infected person. Infected people have spread MERS-CoV to others in healthcare settings, such as hospitals. Researchers studying MERS have not seen any ongoing spreading of MERS-CoV in the community.
All reported cases have been linked to countries in and near the Arabian Peninsula. Most infected people either lived in the Arabian Peninsula or recently traveled from the Arabian Peninsula before they became ill. A few people have gotten MERS after having close contact with an infected person who had recently traveled from the Arabian Peninsula. The largest known outbreak of MERS outside the Arabian Peninsula occurred in the Republic of Korea in 2015 and was associated with a traveler returning from the Arabian Peninsula.
Public health agencies continue to investigate clusters of cases in several countries to better understand how MERS-CoV spreads from person to person.
PREVENTION & TREATMENT
Prevention
There is currently no vaccine to protect people against MERS. But scientists are working to develop one.
You can help reduce your risk of getting respiratory illnesses:
- Wash your hands often with soap and water for at least 20 seconds, and help young children do the same. If soap and water are not available, use an alcohol-based hand sanitizer.
- Cover your nose and mouth with a tissue when you cough or sneeze, then throw the tissue in the trash.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Avoid personal contact, such as kissing, or sharing cups or eating utensils, with sick people.
- Clean and disinfect frequently touched surfaces and objects, such as doorknobs.
TREATMENT
There is no specific antiviral treatment recommended for MERS-CoV infection. Individuals with MERS often receive medical care to help relieve symptoms. For severe cases, current treatment includes care to support vital organ functions.
PEOPLE WHO MAY BE AT INCREASED RISK FOR MERS
· Recent Travelers from the Arabian Peninsula
If you develop a fever and symptoms of respiratory illness, such as cough or shortness of breath, within 14 days after traveling from countries in or near the Arabian Peninsula you should call ahead to a healthcare provider and mention your recent travel. Countries considered in and near the Arabian Peninsula include: Bahrain; Iraq; Iran; Israel, the West Bank, and Gaza; Jordan; Kuwait; Lebanon; Oman; Qatar; Saudi Arabia; Syria; the United Arab Emirates (UAE); and Yemen.
· Close Contacts of an Ill Traveler from the Arabian Peninsula
If you have had close contact with someone within 14 days after they traveled from a country in or near the Arabian Peninsula and the traveler has/had fever and symptoms of respiratory illness, such as cough or shortness of breath, you should monitor your health for 14 days, starting from the day you were last exposed to the ill person.
If you develop fever and symptoms of respiratory illness, such as cough or shortness of breath, you should call ahead to a healthcare provider and mention your recent contact with the traveler.
- Close Contacts of a Confirmed Case of MERS
If you have had close contact with someone who has a confirmed MERS-CoV infection, you should contact a healthcare provider for an evaluation. Your healthcare provider may request laboratory testing and outline additional recommendations, depending on the findings of your evaluation and whether you have symptoms. You most likely will be asked to monitor your health for 14 days, starting from the day you were last exposed to the ill person. Watch for these symptoms:
- Fever. Take your temperature twice a day. Fever may not be present in some patients, such as those who are very young, elderly, immunosuppressed, or taking certain medications. Clinical judgement should be used to guide testing of patients in such situations.
- Coughing
- Shortness of breath
- Other early symptoms to watch for are chills, body aches, sore throat, headache, diarrhea, nausea/vomiting, and runny nose.
If you develop symptoms, call ahead to your healthcare provider as soon as possible and tell them about your possible exposure to MERS-CoV so the office can take steps to keep other people from getting infected. Ask your healthcare provider to call the local or state health department.
Close contact is defined as a) being within approximately 6 feet (2 meters), or within the room or care area, of a confirmed MERS case for a prolonged period of time (such as caring for, living with, visiting, or sharing a healthcare waiting area or room with, a confirmed MERS case) while not wearing recommended personal protective equipment or PPE (e.g., gowns, gloves, NIOSH-certified disposable N95 respirator, eye protection); or b) having direct contact with infectious secretions of a confirmed MERS case (e.g., being coughed on) while not wearing recommended personal protective equipment.
· Healthcare Personnel Not Using Recommended Infection-Control Precautions
Healthcare personnel should adhere to recommended infection control measures, including standard, contact, and airborne precautions, while managing symptomatic close contacts, patients under investigation, and patients who have probable or confirmed MERS-CoV infections. They should also use recommended infection control precautions when collecting specimens.
Healthcare personnel who had close contact with a confirmed case of MERS while the case was ill, if not using recommended infection control precautions (e.g., appropriate use of personal protective equipment), are at increased risk of developing MERS-CoV infection. These individuals should be evaluated and monitored by a healthcare professional with a higher index of suspicion.
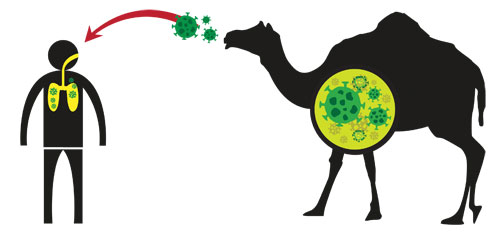
- People with Exposure to Camels
Direct contact with camels is a risk factor for human infection with MERS-CoV.
The World Health Organization has posted a general precaution for anyone visiting farms, markets, barns, or other places where animals are present. Travelers should practice general hygiene measures, including regular handwashing before and after touching animals, and avoiding contact with sick animals. Travelers should also avoid consumption of raw or undercooked animal products. The World Health Organization considers certain groups to be at high risk for severe MERS. These groups include people with diabetes, kidney failure, or chronic lung disease, and people who have weakened immune systems. The World Health Organization recommends that these groups take additional precautions:
- Avoid contact with camels
- Do not drink raw camel milk or raw camel urine
- Do not eat undercooked meat, particularly camel meat
www.cdc.gov/coronavirus/mers/about/index.html
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.