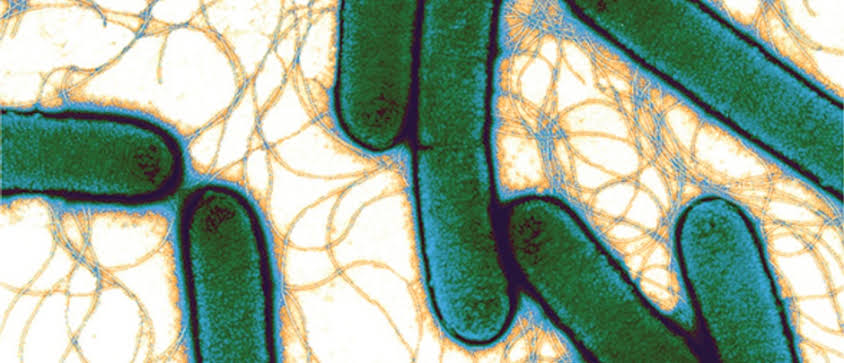
Microorganisms are ubiquitous and are thus found everywhere including the soil. The soil no doubt is inundated with a wide variety of microorganisms including those that are pathogenic to humans, plants and animals and even microbes that are of immense industrial and economic importance to mankind and his environment. For example, the first commercial antibiotic penicillin was originally and naturally sourced from Penicillium species especially P. notatum and P. chrysogenum, which are prominent microbes found in the soil.
The soil is a dwelling place to a wide array of microorganisms including bacteria, protozoa, helminths, fungi and some viruses which cause a handful of disease in humans (Table 1).
Table 1. Microbial diseases transmissible through the soil
| Organism | Disease | Clinical symptoms | Prevention/control/treatment |
| BACTERIAL DISEASES | |||
| Clostridium perfringens | Gas gangrene | Progressive necrotic skin/wound lesion, fever, toxemia, foul-smelling discharge, and shock | Early and adequate cleansing of contaminated wounds and surgical debridement. Administration of penicillin and polyvalent antitoxin are used for treatment. |
| Yersinia enterocolitica | Yersiniosis | Abdominal pain, diarrhea and fever | Conventional sanitary precautions and avoiding contact with animal droppings or feaces. Chloramphenicol, tetracycline and aminoglycoside are used for treatment. |
| Clostridium botulinum | Botulism | Respiratory paralysis and gastrointestinal upset. | Vegetables, fruits and other raw materials for food production should be kept away from soil contamination; and they should be properly washed and cleaned before use. Maintenance of adequate ventilation using mechanical respirator is vital to ensure proper airflow. Antitoxins are administered in cases of botulism. |
| Bacillus anthracis | Anthrax | Symptoms vary with the location of the disease. Fever, malaise, skin oedema, headache and GIT symptoms | Active immunization, use of protective clothing’s when handling infected materials, infected animal carcasses should be burned or buried deeply. Ciprofloxacin, penicillin G and erythromycin are used for treatment. |
| Campylobacter jejuni | Campylobacteriosis | Profuse diarrhea, abdominal pain, fever and malaise | Food should be properly cooked and protected from feacal contamination by animal droppings. |
| Actinomyces israelii | Actinomycetoma | Swollen, erythematous process in the jaw area, cough, mild fever and purulent sputum | Administration of erythromycin and clindamycin as well as prolonged administration of penicillin is used for treatment. |
| Clostridium tetani | Tetanus | Generalized muscular spasm especially lockjaw trismus | Piercing of the skin especially with sharp objects should be followed with active immunization with tetanus toxoids. And antibiotics (e.g. penicillin) should be administered in cases of wound infection. |
| Listeria monocytogenes | Listeriosis | Intrauterine sepsis and bacteraemia | Ampicillin, sulphamethoxazole-trimethoprim and erythromycin are used for treatment. |
| Leptospira interrogans | Leptospirosis | Jaundice, haemorrhage, and lesions of the eye, skin and | Exposure to feacally contaminated soil should be prevented; and workers who come in regular contact with soil such as farmers, sewer workers and miners should always do so in their protective clothing. Doxycycline is used for treatment. |
| Coxiella burnetii | Q fever | Nausea, headache, vomiting, myalgia, diarrhea, myalgia, abdominal and/or chest pain and non-productive cough | Chloramphenicol, tetracycline, and sulphonamides. |
| Borrelia burgdorferi | Lyme disease | Fever, chills, headache, and malaise | Prevention of the lyme disease is based on avoiding exposure to ticks and lice especially during delousing of furniture’s and other dust-ridden materials. |
| Francisella tularensis | Tularemia | Joint stiffness, muscle pain, malaise, headache and chills | Avoidance of soil contaminated with animal droppings is a key preventive measure. Tetracycline, streptomycin or gentamicin is used for treatment. |
| FUNGAL DISEASES | |||
| Organism | Disease | Clinical symptom | Prevention/control/treatment |
| Aspergillus species | Aspergillosis | Symptoms vary with the type of aspergillosis in a patient. Allergic skin reactions, dyspnea, fatigue, weight loss, and fever | Exposure to conidia of the microbe should be avoided. And itraconazole, amphotericin B and surgery (in some cases) are used for treatment. |
| Blastomyces dermatitidis | Blastomycosis | Chronic pneumonia, myalgias, malaise, night sweats and fever | Avoid inhalation of dust particles (because they may contain the conidia of the organism) and contact with animal droppings especially those of dogs. Amphotericin B and itraconazole are used for treatment. |
| Coccidioides immitis | Coccidioidomycosis | Chronic but progressive pulmonary disease. Arthralgia, malaise, fever, headache and cough | Reducing dust, paving of airfields and road, and planting of grasses and using oil sprays on exposed soils are some preventive/control measures. Amphotericin B, itraconazole and fluconazole are effective for treatment. |
| Histoplasma capsulatum | Histoplasmosis | Coughing up blood, fever, chills, neck stiffness, mouth sores, skin lesions and chest pains | Avoid exposure to dust and wind. Dust usually contain conidia of the organism; and people who work in occupations where dusts are raised should always were protective face masks to avoid the inhalation of dust particles which is likely to contain conidia of H. capsulatum. Itraconazole and amphotericin B are used for treatment. |
| Sporothrix schenckii | Sporotrichosis | Development of red lump at the site of infection, facial lesions, necrotic ulcerative lesions | Prevention includes measures to reduce accidental introduction of the conidia into the body. Woods should be treated with fungicides to avoid aerosolization of spores. Itraconazole and amphotericin B is used for treatment. |
| Pseudallescheria boydii | Mycetoma | Suppuration and abscess formation in subcutaneous tissues of the lower extremities of the hands and feet | Wounds should be properly cleaned and avoid contact with soil during the process of healing. People who work in occupations that involve direct contact with the soil should always wear protective clothing and foot wears to avoid contracting the agent form the soil. Amphotericin B, itraconazole and ketoconazole are used for treatment. |
| Rhizopus species and Mucor species | Mucormycosis | Thrombosis, infarction and necrosis due to the germination of the sporangiophores of the causative agent(s) in the nasal carriage of the individual | Mucormycosis is an opportunistic fungal disease or mycoses common in immunocompromised individuals; and the best preventive measure is usually the maintenance of a good immune system. And infection is also common in areas were tornadoes are experienced due to the aerosolization of spores from the soil into the air. Amphotericin B is used for treatment of the disease. |
| VIRAL DISEASES “It is noteworthy that human viruses have no functional biological role within the soil environment; and this is because viruses unlike other microbes only exist and multiply inside a living host cell. Viruses hardly multiply outside a living host cell. However, some viruses such as the polioviruses and Enteroviruses can survive for sometime within the soil environment. For example, Enteroviruses are usually shed in large amount for longer periods of time in the stool of human reservoirs; and the feacal contamination of food, water and other materials by these viruses especially through the soil are common route via which the pathogen is transmitted in human population.” | |||
| Organism | Disease | Clinical symptom | Prevention/control/treatment |
| Enteroviruses (Human enteric viruses) | Enterovirus infection. They cause GIT infections in humans; and they can also infect the central nervous system (CNS) too | Infantile diarrhea, muscle weakness, conjunctivitis and spasm | Enteroviruses can survive for extended periods in the soil environment; and thus prevention/control is largely depended on avoiding unnecessary contact with soil especially those that are feacally contaminated. Contact with human excreta or sewage which is usually in the soil is a common means of contracting the disease agent. Treatment is usually based on the use of antiviral drugs since there is no specific antiviral agent for the treatment of Enterovirus infection in humans. |
| Hantavirus | Hantavirus infection such as hantavirus pulmonary syndrome and haemorrhagic fever with renal syndrome | Flu-like at onset of the disease. Difficulty in breathing, coughing, stomach pain, dizziness, headache and diarrhea. | Human contact with the excreta of infected rodents in the soil is a common means by which the hantavirus infection is spread in human population. And the direct inhalation of aerosolized viral particles especially during tillage of the soil is another common medium of transmission of hantavirus. Thus, protective face mask should be worn by people who work in occupations where dust particles are easily aerosolized such as in road construction and farming. Avoidance of contact with the droppings of rodents is vital to the prevention/control of hantavirus infection. Ribavirin is usually used for treatment. |
| PROTOZOAL DISEASES | |||
| Organism | Disease | Clinical symptom | Prevention/control/treatment |
| Entamoeba histolytica | Amoebiasis | Symptoms of amoebiasis vary depending on the site of the infection and the intensity of the lesion caused. Loss of appetite, weight loss, abdominal cramp, diarrhea, nausea and vomiting | Since asymptomatic carries of Entamoeba histolytica are usually the main source of contamination and such persons release the cysts of the parasite in their excreta which may contaminate the soil via indiscriminate defecation and sewage leakage, it is vital to improve environmental sanitation to avoid contamination. Sewage and human feacal matter should not be used as organic manure in crop cultivation. Metronidazole or flagyl is the commonest drug used to treat amoebiasis. |
| Balantidium coli | Balantidiasis | Severe fluid loss, watery and bloody stooling, weight loss, abdominal pain, headache, vomiting, headache, fever and loss of appetite | Ingestion of viable cysts of B. coli passed via the stool of pigs and humans is usually the commonest route of contamination. Cysts of B. coli can be ingested via food especially in slaughter houses where feacal contamination of food is possible. Improvement on environmental sanitation reduces the contamination of the infection. Metronidazole and oxytetracycline are usually used for treatment. |
| Cryptosporidium parvum | Cryptosporidiosis | Abdominal cramp, nausea and low-grade fever | Ingestion of feacally contaminated food or water (especially human and animal excreta) is a common source of contamination with C. parvum. Farmers who come in contact with animal excreta are also at risk of contamination. Thus, avoidance of animal excreta especially in feacally-contaminated soil is vital to the prevention and control of the disease. The disease is usually self-healing especially in individuals with strong immunity. However, antiprotozoal agents can be administered to immunocompromised individuals with the infection. |
| Cyclospora cayetanensis | Cyclosporiasis | Weight loss, malaise, abdominal cramp and fatigue | The disease is caused by the ingestion of cysts of the parasites via food or water. Thus, food and raw materials for food production should be preserved and protected from feacally-contaminated soil. Bed rest is recommended in mild cases of the disease. Sulphamethoxazole-trimethoprim and ciprofloxacin are usually administered for treatment especially in severe cases and in immunocompromised patients. |
| Girdia lamblia | Girdiasis | Vomiting, diarrhea, abdominal cramp, malaise and flatulence | Ingestion of feacally-contaminated water or food is a common route via which the disease is spread. Avoidance of feacal-contamination of these products is important to the prevention/control of the disease. Metronidazole or flagyl are used for treatment, but treatment is only recommended for asymptomatic individuals i.e. patients who show clinical signs of the disease. |
| Isospora belli | Isosporiasis | Myalgia, headache, offensive smelling diarrhea, abdominal cramp, low-grade fever and loss of appetite | The disease like cyclosporiasis is caused by the ingestion of cysts of the parasites via food or water. Thus, food and raw materials for food production should be preserved and protected from feacally-contaminated soil. Bed rest is recommended in mild cases of the disease. Sulphamethoxazole-trimethoprim and ciprofloxacin are usually administered for treatment especially in severe cases and in immunocompromised patients. |
| Toxoplasma gondii | Toxoplasmosis | Lymphadenopathy (swollen lymph nodes), dyspnea and non-productive cough | Human contact with the droppings or feaces of domestic animals including cats should be avoided as a measure of prevention/control. Sulphamethoxazole-trimethoprim, clindamycin and pyrimethamine are used for treatment. |
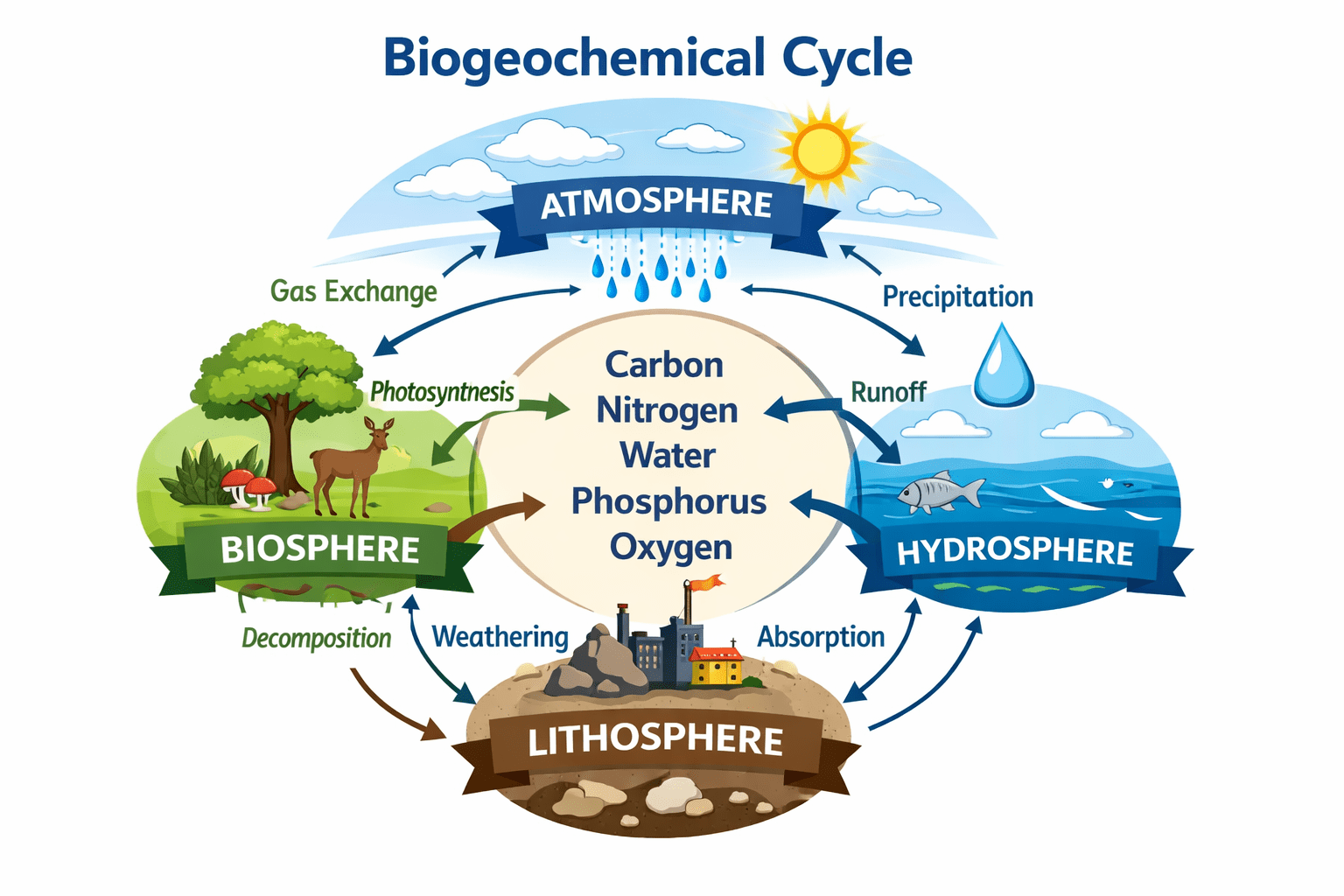
It is a multilayered surface of the earth crust made up of mineral and organic constituents that harbours a huge biodiversity of life that supports several biological processes of microorganisms, humans, plants and animals. The microorganisms found in the soil have several biological functions in the soil such as providing support to the ecosystem as well as proving growth support to plants and improvement of the fertility of the soil. The soil is also home to small animals such as rodents, snails and nematodes, and they give mechanical and protective support to plat roots. Microorganisms that are innately found in the soil help in the cycling of nutrients in the ecosystem.
The soil is home to microbes that are of immense economic, health and industrial importance; and several antibiotics and/or antimicrobial agents have their source from microorganisms (especially bacteria and fungi) that dwells in the soil. Though they contain numerous microbes that are beneficial to mankind, animals, plants and the environment, the soil also contain microorganisms which are capable of causing diseases in humans and even in other animals and plants as well. Microbes that are found in the soil and which cause disease in humans and animals are generally known as soil-borne pathogens.
Most of these soil-borne pathogens are opportunistic pathogens, and they take advantage of the immune system status of susceptible individuals especially people who are immunocompromised (e.g. AIDS patients) to cause infection or disease. Soil-borne pathogens are able of surviving for long periods of time within the soil environment until they find a suitable human host to infect. Human infections with soil-borne pathogens is usually common amongst people who come into direct contact with contaminated soil especially soil contaminated with feacal matter of animal and human origin.
References
Abrahams P.W (2006). Soil, geography and human disease: a critical review of the importance of medical cartography. Progress in Physical Geography, 30:490-512.
Baumgardner D.J (2012). Soil-related bacterial and fungal infections. J Am Board Fam Med, 25:734-744.
Maier R.M, Pepper I.L. and Gerba C.P (2000). Environmental Microbiology. Academic Press, San Diego.
Miguel A, Manuel F, Francisco J.P and Antonio B (2006). Environmental biocatalysis: from remediation with enzymes to novel green processes. TRENDS in Biotechnology, 24(6):1-7.
Mishra B.B, Nanda D.R and Dave S.R (2009). Environmental Microbiology. First edition. APH Publishing Corporation, Ansari Road, Darya Ganj, New Delhi, India.
Paul E.A (2007). Soil Microbiology, ecology and biochemistry. 3rd edition. Oxford: Elsevier Publications, New York.
Pelczar M.J Jr, Chan E.C.S, Krieg N.R (1993). Microbiology: Concepts and Applications. McGraw-Hill, USA.
Pelczar M.J., Chan E.C.S. and Krieg N.R. (2003). Microbiology of Soil. Microbiology, 5th Edition. Tata McGraw-Hill Publishing Company Limited, New Delhi, India.
Pepper I.L and Gerba C.P (2005). Environmental Microbiology: A Laboratory Manual. Second Edition. Elsevier Academic Press, New York, USA.
Roberto P. Anitori (2012). Extremophiles: Microbiology and Biotechnology. First edition. Caister Academic Press, Norfolk, England.
Salyers A.A and Whitt D.D (2001). Microbiology: diversity, disease, and the environment. Fitzgerald Science Press Inc. Maryland, USA.
Sawyer C.N, McCarty P.L and Parkin G.F (2003). Chemistry for Environmental Engineering and Science (5th ed.). McGraw-Hill Publishers, New York, USA.
Ulrich A and Becker R (2006). Soil parent material is a key determinant of the bacterial community structure in arable soils. FEMS Microbiol Ecol, 56(3):430–443.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.