Superficial mycoses are fungal infections which are only limited to the keratinized outer layer of the skin, hair and nails. Superficial mycoses unlike other forms of mycoses rarely result in inflammatory reactions in the host but it is usually characterized by intense itching and peeling or scaling of the affected body sites. They are self-limiting mycoses and benign in their action. Superficial mycoses are non-systemic fungal infections that only infect the surface layer of the skin, and they are usually associated to poor personal hygiene amongst people.
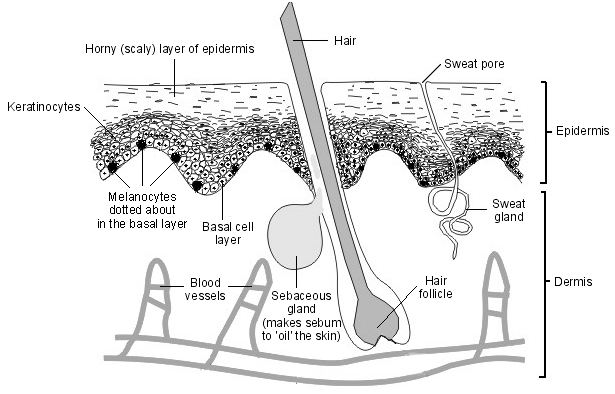
Fungal organisms that cause superficial mycoses are the least known penetrating or invasive fungal species that cause mycoses in humans (Table 1). This is because they only colonize the keratinized outer layer of the skin especially the malpighian layer of the epidermis- which contains keratinocytes that produces the protein keratin, and they generally have no systemic or invasive effect on the body during or after prior infection with the causative agents.
Superficial mycoses are contagious mycoses, and thus it can be transferred or spread in a defined human population via direct body contact with infected persons. People who share personal items of infected individuals such as bathing soap and towels or bed sheaths are at risk of catching superficial mycoses. Though most superficial mycoses are self-limiting and can heal on their own even without formal treatment, they can best be treated through a careful removal of the affected scalp of the skin or infected hairs and nails.
Subcutaneous mycosis is common amongst children, adolescents and young people who may occasionally experience some level of poor personal hygiene in their lifetime especially during their early development. However, the disease is normally localized in underdeveloped or developing countries especially in places where personal and public hygiene is poor; and both children and adults are easily infected. Topical antifungal agents can be applied in some cases to hasten the healing process of the infection and thus inhibit fungal growth in the affected body sites.
Table 1. Synopsis of superficial mycoses
| Mycoses | Causative agent | Clinical feature | Site of infection |
| Black piedra | Piedraia hortai | Black piedra is a chronic but mild fungal infection characterized by the adherence of hard black nodules to infected hairs especially at the hair shaft. | Hairs of the scalp |
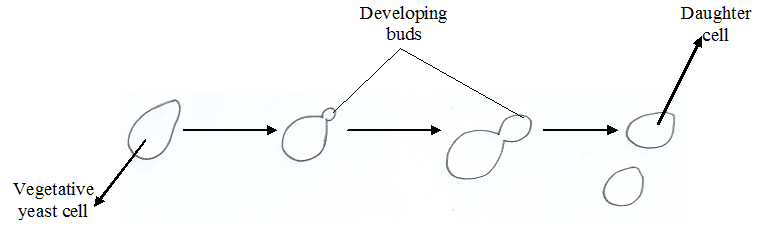
| White piedra | Trichosporon beigelii | White piedra unlike black piedra is characterized by the adherence of soft & gelatinous larger white nodules to infected hairs including those of the pubic regions, scalp and beard. Arthroconidia are usually present in the hair shaft of affected hairs. | Hairs of the scalp, pubic region and beard |
| Pityriasis or Tinea versicolor | Malassezia species | Pityriasis versicolor is a chronic but mild fungal infection characterized by the invasion of the skin especially the cornified layer. There is also production of pigmented macula on the skin especially at the chest and back regions. | Face, back, chest and arms |
| Tinea nigra | Hortaea (Exophiala) werneckii | Tinea nigra is a chronic but asymptomatic fungal infection of the stratum corneum (i.e. the layer of dead keratinized cells of the epidermis which progressively falls off). It is characterized by brown to black discolouration of the outer skin layer especially those of the palms. | Palm |
References
Anaissie E.J, McGinnis M.R, Pfaller M.A (2009). Clinical Mycology. 2nd ed. Philadelphia, PA: Churchill Livingstone Elsevier. London.
Beck R.W (2000). A chronology of microbiology in historical context. Washington, D.C.: ASM Press.
Black, J.G. (2008). Microbiology: Principles and Explorations (7th ed.). Hoboken, NJ: J. Wiley & Sons.
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA.
Brown G.D and Netea M.G (2007). Immunology of Fungal Infections. Springer Publishers, Netherlands.
Calderone R.A and Cihlar R.L (eds). Fungal Pathogenesis: Principles and Clinical Applications. New York: Marcel Dekker; 2002.
Chakrabarti A and Slavin M.A (2011). Endemic fungal infection in the Asia-Pacific region. Med Mycol, 9:337-344.
Champoux J.J, Neidhardt F.C, Drew W.L and Plorde J.J (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases. 4th edition. McGraw Hill Companies Inc, USA.
Chemotherapy of microbial diseases. In: Chabner B.A, Brunton L.L, Knollman B.C, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, McGraw-Hill; 2011.
Chung K.T, Stevens Jr., S.E and Ferris D.H (1995). A chronology of events and pioneers of microbiology. SIM News, 45(1):3–13.
Germain G. St. and Summerbell R (2010). Identifying Fungi. Second edition. Star Pub Co.
Ghannoum MA, Rice LB (1999). Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev, 12:501–517.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Larone D.H (2011). Medically Important Fungi: A Guide to Identification. Fifth edition. American Society of Microbiology Press, USA.
Levinson W (2010). Review of Medical Microbiology and Immunology. Twelfth edition. The McGraw-Hill Companies, USA.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of Microorganisms, 12th edition. Pearson Benjamin Cummings Inc, USA. Mahon C. R, Lehman D.C and Manuselis G (2011). Textbook of Diagnostic Microbiology. Fourth edition. Saunders Publishers, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.