Staphylococcus aureus is a Gram-positive, coagulase-positive, catalase-positive, non-motile coccus found in the genus Staphylococcus and family Staphylococcaceae. They are facultative anaerobic organisms, and they cause haemolysis on blood agar. Staphylococcus species are usually arranged in groups, in pairs, tetrads and they also occur singly. S. aureus usually appear as grapelike clusters under the microscope. They are asporogenous or non-sporulating in nature. Asporogenous bacteria are organisms that do not produce spores. S. aureus are habitually found in the nose of humans but it may be found regularly in most other anatomical sites of the body such as the respiratory tract, mucous membranes, GIT and skin.
They can also be found on fomites including tables, clothing materials, and bed linens. Out of all the species of Staphylococcus, only Staphylococcus epidermidis (normal flora of the human skin) and S. aureus are more clinically important to humans. S. aureus normally exist as either resident or transient microorganisms on the human skin. In the microbiology laboratory, S. aureus can easily be isolated by taking samples from the nose and skin of volunteers and culturing same on growth/bacteriological culture media.
It is noteworthy that a good percentage of healthy individuals carry S. aureus in their nose, and these persons can be infectious to susceptible hosts by transferring the microbe via their hands (after picking their noses) or through body contacts. S. aureus cause gastroenteritis; and they can also colonize the female vagina especially during menstruation to cause infection. Thus, most infections of S. aureus are due to poor personal and environmental hygiene.
S. aureus causes a variety of infections/diseases in humans and these include abscesses, wound infections, gastroenteritis, toxic shock syndrome toxin (TSST) disease, pneumonia, burns, and septicaemia. S. aureus produce a range of enzymes and toxins which aids in its pathogenicity or disease course. S. aureus is mostly implicated in human pyogenic infections such as boils, pimples, impetigo and pustules.
PATHOGENESIS OF STAPHYLOCOCCUS AUREUS INFECTION
S. aureus is notorious in causing a variety of invasive and mixed infections in humans including pus-forming infections, food-poisoning (gastroenteritis) characterized by vomiting, skin infections and blood-borne related diseases. Urinary tract infections (UTIs), pneumonia, mastitis, endocarditis, meningitis and osteomyelitis are some of the serious infections or diseases in which S. aureus is implicated as a causative agent. S. aureus is also amongst the causative agents implicated in most nosocomial infections especially postoperative wound infections.
Community-acquired methicillin resistant S. aureus (CA-MRSA) and hospital-acquired methicillin resistant S. aureus (HA-MRSA) are other important infections caused by resistant strains of pathogenic S. aureus. It is noteworthy that only pathogenic S. aureus strains are invasive in nature, haemolytic and coagulase-producing; and they are largely responsible for the multitude of infections caused by Staphylococcus species. Non-pathogenic Staphylococcus species such as S. epidermidis amongst others are noninvasive, non-haemolytic and they do not produce coagulase enzymes.
The invasiveness of S. aureus, virulence and pathogenicity is founded on the ability of the pathogen to produce a variety of toxins and extracellular enzymes that determine the course of the infection. These toxins and enzymes produced by the microbe help to increase the severity of infection during S. aureus invasion. In general, the virulence and/or pathogenicity of pathogenic S. aureus are largely dependent on the invasiveness of the invading strain, and the shared or cooperative action of the toxins and extracellular enzymes they produce. Thus the pathogenesis of S. aureus will be expanded here based on the virulence factors (i.e. enzymes and toxins) that they produce.
EXFOLIATIN FROM S. AUREUS
Exfoliatin or exfoliative toxins (ET) are protein toxins produced by Staphylococcus aureus strains that cause staphylococcal scalded skin syndrome (SSSS) in humans. Two serological types of exfoliative toxins are known, and they are ETA (a chromosomally-mediated toxin) and ETB (a plasmid-mediated toxin). ETA is heat-stable while ETB is a heat-labile toxin; and both toxins exhibit esterase and protease activity that have an impact on the integrity of the skin. SSSS is a staphylococcal disease caused by the plasmid-mediated toxin (ETB) produced by S. aureus; and it is clinically experienced as a desquamation of the upper skin layer.
In SSSS, there is usually a broad loss of the epidermis (a condition known as epidermolysis), and this exposes the red area beneath the skin surface. SSSS is commonly experienced in neonates and young children below 5 years of age; and the disease can also occur in monkeys and mice but not in rats. Exfoliatin toxins are superantigens; and they are also known as epidermolytic toxins due to their ability to cause an extensive peeling of the human skin (i.e. a loss of the skin’s epidermis). They are also implicated in causing staphylococcal impetigo disease in humans.
TOXIC SHOCK SYNDROME TOXIN-1 (TSST-1)
Toxic shock syndrome toxin-1 (TSST-1) is another class of superantigens produced by S. aureus, and it causes toxic shock syndrome disease in humans. In toxic shock syndrome disease, there is a profound release of staphylococcal superantigens into the bloodstream of the infected individuals and this leads to toxaemia (i.e. a medical condition in which there is high amounts of toxins in the blood). Patients suffering from toxic shock syndrome disease usually experience skin desquamation (Figure 1), and this can progress throughout the body just like in SSSS. Toxic shock syndrome disease is a fatal and severe disease characterized clinically by widespread desquamated skin rash, vomiting, muscle ache, high fever and diarrhea; and renal and hepatic injury in some complicated cases.
Young children and women who use certain types of tampons during their menses are mostly affected by the disease. Toxic shock syndrome disease can also be experienced in non-menstruating women and men who may have other infections e.g. wound infections. Specifically, TSST-1 stimulates massive production of cytokines (e.g. interleukins, tumour necrosis factor, and interferons) without the availability of any processed antigen to attack, and this result in toxic shock due to toxaemia. People without the appropriate neutralizing antibody against TSST-1 have recurrence of toxic shock syndrome disease.

ENTEROTOXINS FROM S. AUREUS
Enterotoxins are superantigens produced by pathogenic S. aureus strains that cause toxicoses, a type of food poisoning in humans. The enterotoxins of S. aureus are designated as A, B, C, D, and E proteins; and they are notorious in stimulating massive production of cytokines that cause staphylococcal food poisoning in humans who consume contaminated food. Produced or preformed in food, staphylococcal enterotoxins are plasmid-mediated and chromosomally-mediated, and some are phage-borne (e.g. enterotoxin A).
Staphylococcal enterotoxins can also be produced by pathogenic S. aureus in the intestinal tract of infected humans. Enterotoxins of pathogenic S. aureus are genetically related to TSST-1, and both share many characteristics together but enterotoxins are more heat-stable and resistant to enzymes in the digestive tract of affected people. Staphylococcal food poisoning is usually characterized by non-bloody diarrhea, abdominal cramp and vomiting (emesis). Enterotoxins like TSST-1 stimulate massive production of cytokines that activate the vomiting centre in the brain and cause gastroenteritis.
STAPHYLOCOCCAL ALPHA (α) TOXIN FROM S. AUREUS
Staphylococcal alpha (α) toxins are cytolytic toxins produced by pathogenic S. aureus, and which has killing effect on the cell membranes of eukaryotic cells. They are the most potent membrane-damaging haemolysins produced by S. aureus, and they basically act on a wide variety of cell membranes where they cause haemolysis and necrosis. Alpha toxins cause lysis by producing small pores or holes in the cell membranes of cells (e.g. erythrocytes), thus leading to the massive loss of cell materials from the damaged cells.
STAPHYLOCOCCAL BETA (β) TOXIN FROM S. AUREUS
Staphylococcal beta (β)toxins are less cytotoxic than α toxin but they also attack erythrocytic cells and some cells of the nerves (e.g. sphingomyelin). Beta toxins have high affinity for lipid-rich cells where they cause haemolysis.
STAPHYLOCOCCAL GAMMA (γ) TOXIN FROM S. AUREUS
Staphylococcal gamma (γ) toxins are produced by both S. aureus and S. epidermidis. Gamma toxins disrupt the integrity of cell membranes like the other haemolysins produced by S. aureus.
LEUKOCIDIN FROM S. AUREUS
Leukocidin is a cell membrane damaging toxin produced by pathogenic strains of S. aureus. They specifically kill leukocytes by creating small pores or holes that increases loss of materials from the damaged cell, thus inhibiting the process of phagocytosis in the infected human host. Panton-valentine (P-V) leukocidin as they are often called are haemolytic in nature, and they are mostly implicated in the majority of resistant Staphylococcus aureus infections (e.g. methicillin resistant Staphylococcus aureus, MRSA).
EXTRACELLULAR ENZYMES PRODUCED BY S. AUREUS
- Catalase: Catalase is an enzyme produced by pathogenic S. aureus, and it inhibits the process of phagocytosis. It enhances the survival of the pathogen in phagocytes through the production of the enzyme. Catalase enzyme production is used for the biochemical identification of S. aureus in the laboratory, and it converts hydrogen peroxide (H2O2) to water and oxygen; thereby walling off or protecting the infected body sites from phagocytic cells.
- Proteases: Proteases or proteinases are extracellular enzymes produced by pathogenic S. aureus, and which assist the pathogen in breaking down protein molecules.
- Nuclease: Nuclease enzymes produced by pathogenic S. aureus breaks down nucleic acids of infected cells in human host. DNase enzymes produced by pathogenic S. aureus perform a similar function with nucleases in that they destroy the host cell DNA.
- Beta-lactamase: Beta lactamase enzymes produced by pathogenic S. aureus are of clinical significance in that this class of enzymes confers on the pathogen the capacity to develop resistance to a range of synthetic antibiotics and other antimicrobials. Beta lactamase enzymes of pathogenic S. aureus degrade beta-lactam antibiotics such as penicillins.
- Lipase: Lipases are fat or lipid destroying enzymes produced by pathogenic S. aureus.
- Coagulase: Pathogenic S. aureus produces coagulase enzymes, and this characteristic differentiates them from non-pathogenic S. aureus strains which do not produce coagulase. The production of this enzyme by pathogenic S. aureus strains inhibits the process of phagocytosis in the affected human host cells. Coagulase enzymes converts fibrinogen to fibrin clot which surrounds and protect infected sites from the action of phagocytes. The production of coagulase (blood clotting factor) is used to identify pathogenic S. aureus in the clinical microbiology laboratory.
- Staphylokinase: Staphylokinase is an extracellular enzyme produced by pathogenic S. aureus, and it is a plasminogen activator (i.e. the enzyme stimulates a plasmin-like proteolytic activity that lyses fibrin). Streptokinase may aid in the spreading of the pathogen within the host due to its ability to degrade fibrin clots.
- Hyaluronidase: Hyaluronidase is an enzyme that breaks down hyaluronic acid that makes up the host connective tissues. The ability of pathogenic S. aureus to produce hyaluronidase encourages the spread of the pathogen in host tissues.
- Protein A: Protein A is found in the cell wall of most S. aureus strains, and they prevent the activation of complement in the host cell. Anti-phagocytic in nature, protein A binds to the crystallizable fragment (Fc portion) of antibody molecules (e.g. IgG), and thus prevents phagocytosis and opsonization. In this way, protein A (staphylococcal surface protein) contributes to the virulence of pathogenic S. aureus.
LABORATORY DIAGNOSIS OF STAPHYLOCOCCUS AUREUS INFECTION
The laboratory diagnosis of staphylococcal disease is based mainly on the isolation and identification of the invading pathogen through microscopy and culture. Serological and biochemical tests (e.g. catalase, DNase and coagulase tests) are also employed in typing the strain of S. aureus implicated in the disease process. Blood, CSF, sputum, tracheal aspirate, pus, and surface swab specimens from infected sites (e.g. wound and burns) are clinical specimens collected for laboratory investigations.
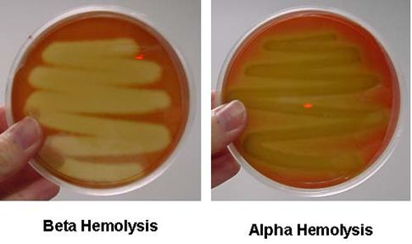
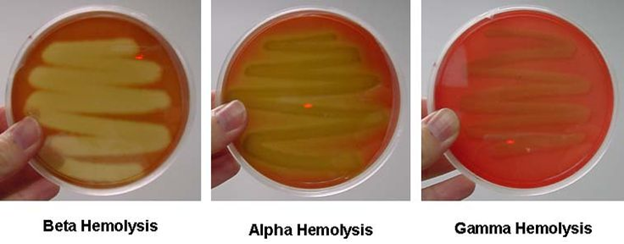
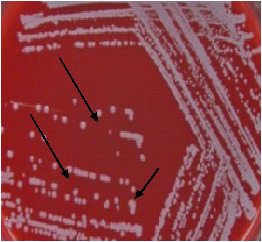
Gram staining reveals Gram-positive grape-like cocci in clusters, tetrads or pairs under the microscope. Mannitol salt agar (MSA) is a selective medium (that contains NaCl which inhibit other normal flora and non-staphylococcal organisms) used to screen for S. aureus and recover the pathogen from specimens resulting from a mixed infection. S. aureus produces several types of haemolysis including beta-haemolysis, alpha haemolysis and gamma haemolysis on blood agar media (Figure 2). S. aureus can also be cultured and isolated successfully on blood agar producing white or pale haemolytic colonies (Figure 3), chocolate agar and MacConkey agar. S. aureus grow aerobically at 35-37oC.
IMMUNITY TO STAPHYLOCOCCUS AUREUS INFECTION
Host defense against staphylococcal diseases or infections is based on the action of phagocytic cells against invading pathogens. Though phagocytosis plays active role in inhibiting the progression of the infection, pathogenic S. aureus is ingenious in producing toxins and extracellular enzymes that disrupts the course of action of phagocytes. No active immunity is developed in the host against a futuristic staphylococcal infection.
TREATMENT OF STAPHYLOCOCCUS AUREUS INFECTION
Therapy for staphylococcal disease is based on the administration of specific class of antibiotics to which the pathogen is susceptible to. All isolated Staphylococcus species should be subjected to antimicrobial susceptibility studies so as to guide treatment. Though S. aureus is resistant to some known potent antibiotics, cephalosporins, vancomycin, methicillin, oxacillin and penicillins are some of the drug of choice used for treating staphylococcal disease or infections.
Strains of S. aureus resistant to methicillin, penicillin and vancomycin now exist in both the community and hospital environment. Drainage of the fluids or pus in abscess caused by S. aureus can be employed in the management of pus-infections mediated by the pathogen. Staphylococcal food poisoning should be treated through fluid and electrolyte replacement by the administration of the correct amount of a salt-sugar-solution (SSS) to the affected patients since the disease normally leads to a considerable loss of fluid from the body.
PREVENTION AND CONTROL OF STAPHYLOCOCCUS AUREUS INFECTION
Staphylococcus species are habitual inhabitants of the human body especially the nares and skin where they are resident as normal microflora. Most individuals who harbour pathogenic S. aureus are asymptomatic, and they shed the pathogen to susceptible hosts around them. The control and prevention of staphylococcal infections in the hospital environment should be based on the practice of proper hospital infection control measures.
No vaccine currently exist to prevent staphylococcal diseases or infections, thus it is vital for individuals and hospital institutions to maintain and imbibe personal hygienic practices such as hand washing. Doctors, nurses and other health personnel should maintain aseptic technique as they do their job especially around newborn wards and operating rooms. Wounds and burns should be properly dressed and disinfected with antiseptics too.
The removal of superabsorbent tampons from general circulation has helped to reduce the incidence of toxic shock syndrome disease in menstruating women. Contaminated foods should be avoided; and food handlers should always observe proper hygiene in the handling, preparation and distribution of food in order to avoid the outbreak of food poisoning due to Staphylococcus aureus.
OTHER SPECIES OF STAPHYLOCOCCI
- S. saprophyticus:S. saprophyticus is a common cause of community acquired urinary tract infection. It is a leading cause of cystitis in young women; and it is second only to E. coli as the most frequent causative organism of uncomplicated UTI in women. It is found as a normal flora in the female genital tract and perineum; and S. saprophyticus is also found in the vegetables and the environment and in the gastrointestinal tract of animals.
- S. epidermidis:S. epidermidis is part of the human normal flora, and it is abundantly found on the skin. It is not pathogenic in nature but it can cause infection in immunocompromised patients. S. saprophyticus is an opportunistic bacterium that requires a breach in the host’s innate defenses to cause infection.
- S. saccharolyticus:S. saccharolyticus causes infective endocarditis; and it is known to contaminate samples of platelets taken from humans.
- S. lugdunensis: S. lugdunensis is a common cause of skin and soft tissue infections in the community. It occurs as a normal flora on human skin, but it has been recorded as a cause of serious human infections including osteomyelitis, arthritis, septicaemia, wound infections, and aggressive endocarditis.
- S. warneri:S. warneri is found on the skin of humans and animals as a normal flora. It rarely causes disease in humans, but it may occasionally cause infection in patients whose immune system is compromised.
- S. intermedius:S. intermedius is isolated from the anterior nares of pigeons, dogs, mink, and horses. It is a part of the normal flora in the oral cavity, upper respiratory tract, female urogenital tract and gastrointestinal tracts; and it can be found in human feaces. S. intermedius is an opportunistic organism that can cause infection in compromised human hosts.
- S. capitis: S. capitis is a coagulase-negative species of Staphylococcus. It is part of the normal flora of the skin of the human scalp, face, neck, and ears and it has been associated with prosthetic valve endocarditis.
- S. caprae: S. caprae is implicated in infections of the bloodstream, urinary tract, bones, and joints. It was originally isolated from goats, but it has also been isolated from human samples.
- S. haemolyticus: is an opportunistic organism abundantly found in the axillae, perineum, and inguinal regions as normal flora; and it also colonizes primates and other domestic animals.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.