Shigella dysenteriae is a Gram-negative, lactose-negative, non-motile, facultatively-anaerobic and rod-like bacterium that is responsible for bacillary dysentery (bloody diarrhea) in humans. Biochemically, S. dysenteriae is methyl-red positive (MR +ve), Voges-Proskauer negative (VP -ve), hydrogen sulphide negative (H2S –ve), citrate negative and lysine decarboxylase negative. S. dysenteriae is found in the genus Shigella and family Enterobacteriaceae. The genus Shigella comprises four distinct species- all of which causes shigellosis or bacillary dysentery; and they are S. dysenteriae, S. flexneri, S. boydii, and S. sonnei. S. dysenteriae is the most virulent species of them all, and it is responsible for causing several cases of shigellosis around the world especially in developing countries where hygiene, good housing, sewage management and sanitation is poor.
Antigenically, Shigella has over 40 serotypes or serovars (as is applicable to Salmonella with over 2000 serovars) and these are typed by the somatic cell wall or “O” antigen of the bacteria. Shigella species unlike E. coli and Salmonella species lack flagellar (H) antigens because they are non-motile in nature. Based on the “O” antigen of the organism, Shigella species is classified into four serogroups viz: serogroup A (S. dysenteriae), serogroup B (S. flexneri), serogroup C (S. boydii) and serogroup D (S. sonnei); and these serogroups contain different serotypes and sub-serotypes of Shigella. Shigella species are invasive bacteria that cause a range of gastrointestinal diseases (shigellosis) in humans. There is no animal reservoir for Shigella species.
The bacteria pathogen inhabits the intestinal tract of humans; and this makes the disease a strict human infection. S. dysenteriae is transmitted via the feacal-oral route especially through contaminated water. Person-to-person transmission of the pathogen is also possible via feacally-contaminated hands or fingers. Other Shigella species (e.g. S. sonnei and S. flexneri) cause food-borne infections in humans, and these are usually transmitted via contaminated dairy products (e.g. egg) and food. Drinking and swimming in feacal-contaminated water and the consumption of food contaminated with sewage or feacal matter of infected person’s aids the transmission of the pathogenic bacteria. Waterborne or food borne infections due to Shigella can ensue in a defined human population when people fail to practice good personal and environmental hygiene.
PATHOGENESIS OF SHIGELLA DYSENTERIAE INFECTION
S. dysenteriae and other Shigella species are basically acquired via the feacal-oral route especially through the consumption of contaminated food, vegetables or water and via infected hands, flies or fingers. Only a small amount or dose of Shigella species (e.g. 103 cells) is actually required to initiate an infection unlike in salmonellosis and other enteric infections where a high dosage of the invading bacteria is required to initiate a pathological condition in the host. After oral ingestion of the bacteria pathogen, S. dysenteriae, an intracellular bacterial pathogen penetrates the mucosal area or surfaces of the colon (large intestine) and ileum (small intestine) where it causes inflammatory and ulcerative reactions. Principally, S. dysenteriae is phagocytosed by macrophages after being taken up by the M cells.
They induce apoptosis and are released from the macrophage and then go on to cause pathological changes within the mucosal cells of the ileum and colon which they invade. M cells are cells of the mucosal epithelial region of the GIT (especially the colon and ileum). S. dysenteriae produce virulent factors such as shigatoxin, verotoxins and cytotoxin which enhances its pathogenicity and/or virulence in vivo; and these toxins triggers inflammation within the GIT. However, the most essential property of Shigella species required to initiate watery diarrheal disease is its invasiveness rather than their toxin production. Toxin production only increases the severity of the disease process even though they may not be too essential for disease development in the affected individual.
Also, S. dysenteriae has a low infectious dose (ID50) compared with other enteric bacteria such as Vibrio species with higher ID50, and thus as little as 10-100 Shigella is enough to initiate an infection once ingested into the body. The severity of Shigellae infection is also determined by the strain of the invading bacteria and on the age of the susceptible host (whether elderly or infants). Some strains of Shigella (e.g. S. dysenteriae Type I) are more virulent than the others. The incubation period of the disease after ingestion of Shigellae is between 2-4 days, and after this there is marked dysentery and dehydration in addition to other associated symptoms in infected individuals.
Diarrhea, vomiting, passing out of watery stool (which is usually bloody and may contain pus or mucous), fever and abdominal cramp are signs and symptoms associated with Shigella infection. Acidosis, loss of fluid and electrolyte and death can occur in children and the elderly. Though invasive in nature, Shigella infection is normally restricted within the GIT, and thus systemic infection (i.e. extra-GIT spread of the pathogen within the host body) rarely occurs.
LABORATORY DIAGNOSIS OF SHIGELLA DYSENTERIAE INFECTION
The laboratory diagnosis of shigellosis or bacillary dysentery is usually dependent on the isolation and identification of S. dysenteriae from stool cultures of infected individuals. Several culture media exists for the cultivation and isolation of S. dysenteriae in the microbiology laboratory. Rectal swabs and fresh stool specimens are usually required from Shigella infected individuals for culture and microscopy.
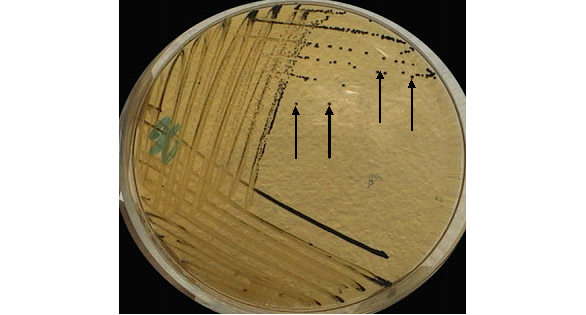
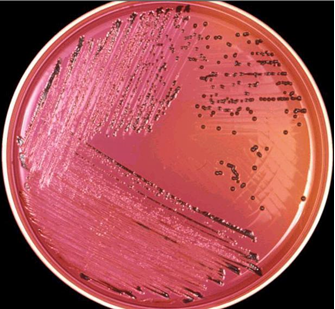
Bacteriologically, S. dysenteriae grow on MacConkey agar (producing non-lactose fermenting transparent colourless-colonies), EMB agar (producing translucent colourless to gold colonies), Salmonella-Shigella agar, SSA (producing opaque colonies) and Hektoen enteric agar (producing green or transparent colonies). Serological tests (e.g. slide agglutination method) and biochemical identification techniques are also available for the identification of the pathogen in the microbiology laboratory. Shigella species cause an alkaline slant and an acid butt on triple sugar iron agar (TSIA) without gas and H2S production.
IMMUNITY TO SHIGELLA DYSENTERIAE INFECTION
Protection against Shigella infection is usually species or strain-specific. This implies that once a person is infected with a particular strain of the organism, that individual is not liable to a re-infection with that same strain of Shigellae. However, infection with a different strain or species of Shigella is still likely in previously Shigella infected people.
TREATMENT SHIGELLA DYSENTERIAE INFECTION
Majority of shigellosis heals spontaneously in about 3-5 days after infection without any formal antibiotic therapy. Sulphamethoxazole-trimethoprim, ciprofloxacin, doxycycline and ampicillin are some of the antibiotics of choice recommended for treating shigellosis. However, antibiotic therapy should only be initiated or administered to severe cases of watery dysentery since the majority of shigellosis are benign in form and may heal spontaneously without antibiotic treatment.
Resistance of some Shigella species to some commonly available drugs (e.g. ampicillin) should be checked via antimicrobial susceptibility testing in order to guide therapy. Fluid replacement is critical for children, infants and the elderly who may have loss massive amounts of fluid due to the watery diarrheal disease.
PREVENTION AND CONTROL OF SHIGELLA DYSENTERIAE INFECTION
Frequent hand washing with soap is critical to the prevention and control of the spread and transmission of Shigella infection since the pathogen is mainly transmitted via feacal-oral route from an infected person to a susceptible individual. Cooked food should be properly covered to prevent flies (which breeds in feacal matter) from perching on it and transmitting the bacteria in the process (i.e. from feaces to food).
Food handlers should practice good personal hygiene and their stool samples should be screened for Shigella species since such persons (when infected) could contaminate food and pass on the pathogen to susceptible human hosts. Outbreak of Shigella infection is common in mental care clinics or hospitals and in day-care facilities or homes where hygiene is poor and feacal-oral spread of the bacteria is common.
Asymptomatic carriers of Shigella (especially amongst food handlers) should be identified, isolated and properly treated with antibiotic therapy. People living in endemic regions should always ensure to get their drinking water from clean sources devoid of any feacal or sewage contamination. Hand washing, proper cooking of food and the practice of good personal and environmental hygiene are important in reducing the morbidity associated with Shigella infection in human population.
OTHER SPECIES OF SHIGELLA
- S. boydii: S. boydii is a nonmotile, non-sporeforming, rod-shaped bacterium in the genus Shigella. It can cause dysentery in humans through fecal-oral contamination.
- S. flexneri: Shigella flexneri is a non-motile, non-spore forming, rod-shaped bacterium that is physiologically similar to Shigella dysenteriae, Shigella boydii, and Escherichia coli. It causes bacterial dysenteries and shigellosis.
- S. sonnei:S. sonnei is a Gram-negative, rod-shaped, nonmotile, non-sporeforming bacterium in the genus Shigella. It is responsible for many cases of shigellosis together with S. flexneri and S. flexneri.It can be transmitted via the feacal-oral route especially through water and food and even through direct body contact.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.