Cutaneous mycoses are fungal infections of the skin, nails and hairs; and they are mainly caused by dermatophytes. While superficial mycoses involves the outermost layers of the skin; cutaneous mycoses generally affects the epidermis layer of the skin i.e. the layer of the skin that underlies the outer skin surface. Cutaneous mycoses can also be called dermatophytoses or dermatomycoses since they are caused by dermatophytes. Dermatophytes are fungi that can degrade the keratinized tissues of living organisms including those of humans and animals.
The outer layer of the human skin is rich in keratin; an insoluble protein molecule produced by keratinocytes and commonly found in hairs, nails and skin scrapings including the feathers and hairs of other animals. Dermatophytes are moulds that mainly attack the non-living or dead keratinized tissues of the human and animal skin. Some of the notable infections caused by dermatophytes in humans include athlete’s foot, jock itch and ringworm or tinea amongst others (Table 1).
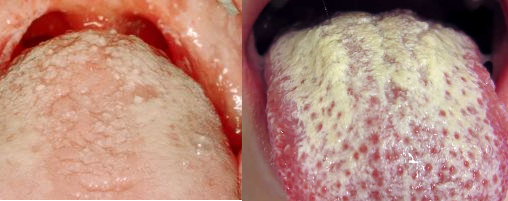
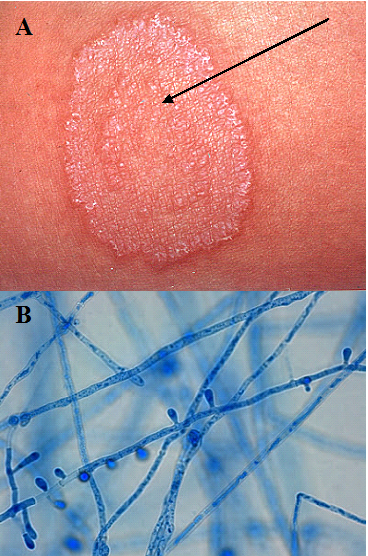
Ringworm or tinea is a communicable fungal infection very common amongst children (Figure 1). Adults are less susceptible to ringworm infection due to the fungistatic action of fatty acids in the sebum produced by their skin; and it is mainly caused by specific fungal genera including Microsporum, Epidermophyton and Trichophyton which are all moulds. Dermatophytes have high affinity for keratinized tissues of the body especially the epidermis of the skin where dead keratinized tissues are located.
Dermatophytes like the fungi that cause superficial mycoses are also among the least invasive fungal organisms because they do not penetrate deep tissues of the body but only colonize the keratinized outer layer of the skin especially the dead layers of the outer skin and other keratinized parts of the body.
Dermatophytes that reside naturally in the soil are known as geophilic fungi (e.g. Microsporum gypseum) while those whose natural habitat is animals such as cattle, horses, dogs and cats are known as zoophilic fungi (e.g. Microsporum species including M. canis, M. gallinae, M. nanum and Trichophyton species including T. verrucosum and T. equinum). Anthropophilic fungi are dermatophytes that naturally reside on the body of humans (e.g. Epidermophyton species and Trichophyton species); and they cause infection following the destabilization of the body’s normal flora.
Cutaneous mycoses are less-debilitating fungal infections even though they are prevalent in most parts of the world; and they are contagious and can spread from person to person via direct body contact with infected persons. Animal-human contacts and the use of personal items of infected individuals such as bathing soaps, bathtub and towels are other predisposing factors to the acquisition of a dermatophyte infection.
Dermatophytoses usually arise following inflammatory activities caused by the invading fungus on the site of infection, and this is normally seen as itching, irritating and erythematous scaling and skin discolouration at affected body sites. Generally, cutaneous mycoses are localized fungal diseases that do not disseminate or spread to other parts of the body, and their name corresponds to the particular site of the body that is affected (Table 1). Dermatophytoses can best be treated with topical and oral antifungal agents.
Table 1. Synopsis of cutaneous mycoses
| Mycoses | Causative agent | Clinical feature | Site of infection |
| Jock itch (Tinea cruris) | Epidermophyton floccosum | Infection usually begins in the skin after trauma or contact with soil or animals harbouring dermatophytes. Tinea cruris is ringworm of the groin region which is normally seen as erythematous scaling at the groin. Infections may start at the scrotum before spreading to the groin; and males are mostly affected with Jock itch. | Groin |
| Tinea barbae | Trichophyton mentagrophytes | Tinea barbae is dermatophytosis of the beard region. It is usually characterized by inflammatory reaction at the beards that may cause pyogenic infection; and the onset of Tinea barbae is initiated after human contact with zoophilic fungi. | Hairs of the beard |
| Nail beds (Tinea unguium) or onchomycosis | Epidermophyton species andTrichophyton species | Tinea unguium or onchomycosis is initiated after nail or foot invasion by zoophilic fungi. Onchomycosis is usually characterized by the discolouration and thickening of the finger & toe nails. | Fingernails and toenails |
| Tinea capitis | Microsporum species and Trichophyton species | Dermatophytosis of the scalp and hair is known as Tinea capitis. Tinea capitis begins following the invasion of the scalp and the hair follicles by the hyphae of zoophilic and anthropophilic fungi. The infection is characterized by the inflammation, scaling & loss of scalp hair. | Scalp hair and head |
| Athlete’s foot or feet (Tinea pedis) | Trichophyton species and Epidermophyton species | Tinea pedis is dermatophytosis of the foot. It is a chronic, acute and ulcerative infection characterized by itching and scaling of the foot or feet especially the tow webs and sole region. Athlete’s foot is the most widespread dermatophytosis of humans; and it is mainly caused by geophilic fungi. | Foot or feet |
| Ringworm (Tinea corporis) | Trichophyton species & Epidermophyton species | Tinea corporis is dermatophytosis of the skin. Ringworm is caused by fungal invasion of the keratinized dead skin layers by anthropophilic fungi. It is usually characterized by advancing red circular patches around the affected skin area. | Skin |
| Tinea manus | Trichophyton species | Dermatophytosis of the fingers is known as Tinea manus. Tinea manus is characterized by itchy lesions that involves one or more fingers; and the infection is caused by zoophilic and anthropophilic fungi. | Fingers |
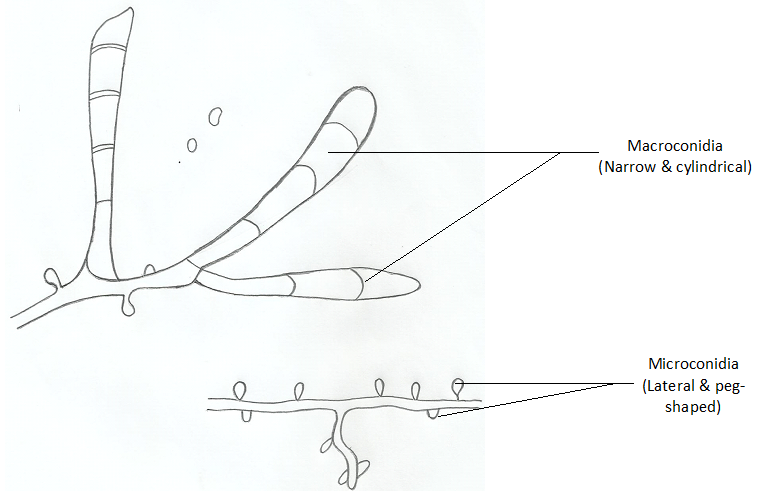
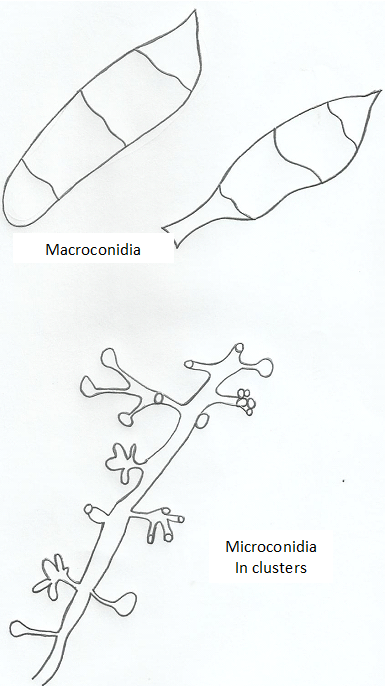
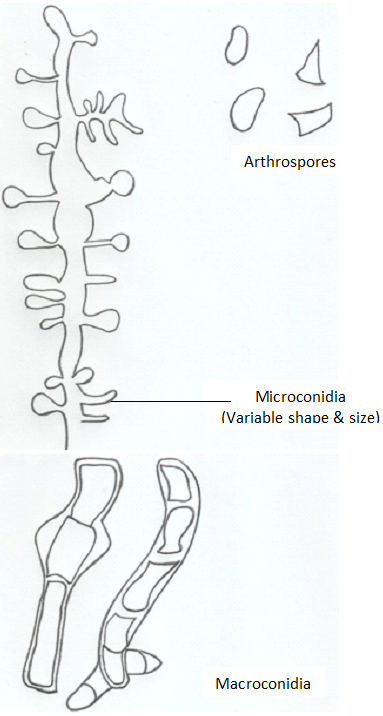
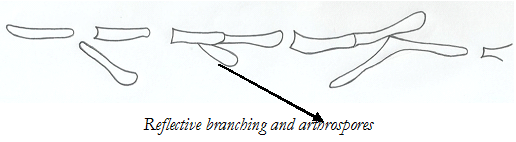
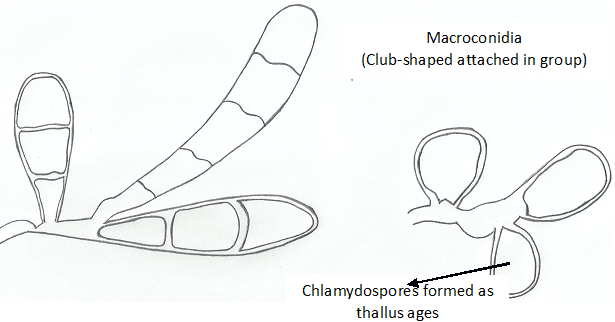
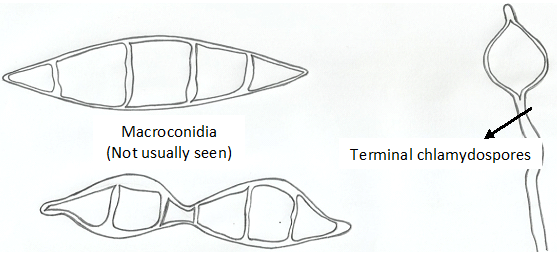
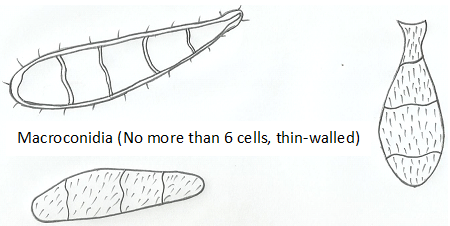
Trichophyton species are spore formers and some notable species that produce both macro- and microconidia include T. rubrum with lateral microconidia and cylindrical macroconidia (Figure 2), T. metangrophytes with macroconidia and clustered grape-like microconidia (Figure 3), T. tonsurans with arthrospores, macroconidia and elongated microconidia (Figure 4), T. soudanensewith reflective and branching arthrospores (Figure 5). Epidermophyton floccosum is unique because it is the only fungal pathogen present in the genus Epidermophyton, and it produces a characteristic macroconidia which is club-shaped and chlamydospores are attached to the fungal thallus (Figure 6). Microsporum species (dermatophytes of the skin and hair) including M. gypseum (Figure 7) and M. audouinii (Figure 8) produce characteristic multicellular macroconidia which aids in their identification.
References
Anaissie E.J, McGinnis M.R, Pfaller M.A (2009). Clinical Mycology. 2nd ed. Philadelphia, PA: Churchill Livingstone Elsevier. London.
Beck R.W (2000). A chronology of microbiology in historical context. Washington, D.C.: ASM Press.
Black, J.G. (2008). Microbiology: Principles and Explorations (7th ed.). Hoboken, NJ: J. Wiley & Sons.
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA.
Brown G.D and Netea M.G (2007). Immunology of Fungal Infections. Springer Publishers, Netherlands.
Calderone R.A and Cihlar R.L (eds). Fungal Pathogenesis: Principles and Clinical Applications. New York: Marcel Dekker; 2002.
Chakrabarti A and Slavin M.A (2011). Endemic fungal infection in the Asia-Pacific region. Med Mycol, 9:337-344.
Champoux J.J, Neidhardt F.C, Drew W.L and Plorde J.J (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases. 4th edition. McGraw Hill Companies Inc, USA.
Chemotherapy of microbial diseases. In: Chabner B.A, Brunton L.L, Knollman B.C, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, McGraw-Hill; 2011.
Chung K.T, Stevens Jr., S.E and Ferris D.H (1995). A chronology of events and pioneers of microbiology. SIM News, 45(1):3–13.
Germain G. St. and Summerbell R (2010). Identifying Fungi. Second edition. Star Pub Co.
Ghannoum MA, Rice LB (1999). Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev, 12:501–517.
Gillespie S.H and Bamford K.B (2012). Medical Microbiology and Infection at a glance. 4th edition. Wiley-Blackwell Publishers, UK.
Larone D.H (2011). Medically Important Fungi: A Guide to Identification. Fifth edition. American Society of Microbiology Press, USA.
Levinson W (2010). Review of Medical Microbiology and Immunology. Twelfth edition. The McGraw-Hill Companies, USA.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of Microorganisms, 12th edition. Pearson Benjamin Cummings Inc, USA.
Mahon C. R, Lehman D.C and Manuselis G (2011). Textbook of Diagnostic Microbiology. Fourth edition. Saunders Publishers, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.