CLOSTRIDIUM TETANI
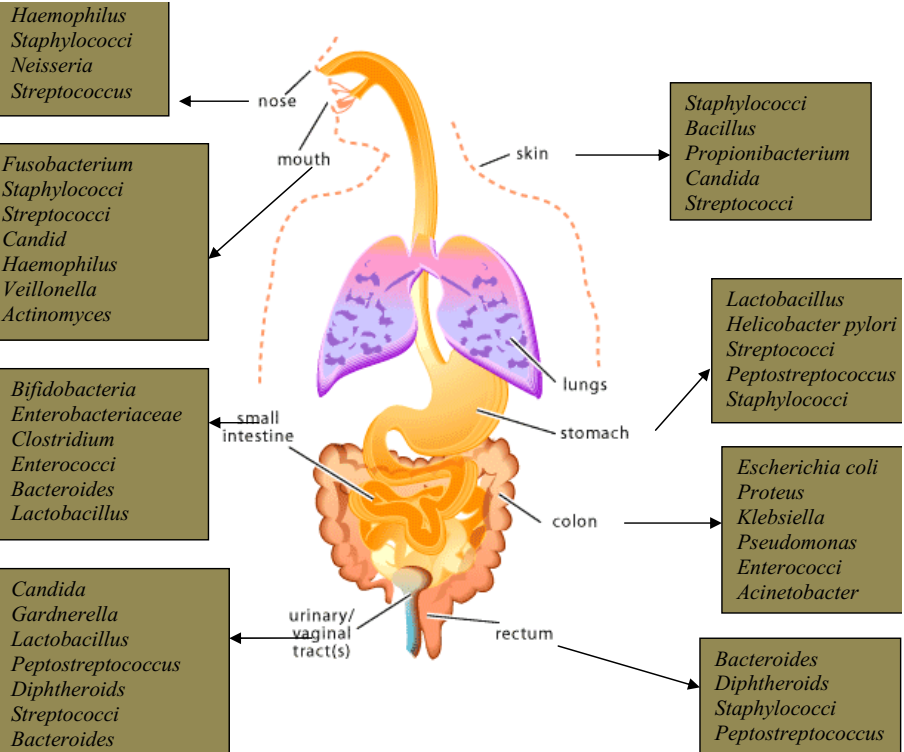
Clostridium tetani is a Gram-positive, motile, anaerobic, spore-forming, rod-shaped bacterium found in the genus Clostridium. It is the main causative agent of tetanus or lock jaw (a non-infectious disease) in humans and animals. Tetanus is an acute localized non-communicable disease of man and animals characterized by muscle spasm and caused by spores of C. tetani that enters the body from the soil via a wound site. C. tetani is ubiquitous in the soil; and can also be found in the hospital environments, feacal matter and intestinal tracts of some animals.
The skin especially a bruised or wounded one is the main portal of entry of C. tetani into the human body.
Human infection begins when spores of C. tetani in the soil enters a wound. The endospore of C. tetani grows and starts producing exotoxins known as tetanospasmin at the site of infection when the wound site is anaerobic and receives low blood or oxygen supply. Tetanospasmin is a plasmid-encoded neurotoxin produced by C. tetani; and it is the main virulence factor of C. tetani infection.
Tetanus toxin (tetanospasmin) has a molecular weight of 150,000 (or 150 kDa) that usually comprises two peptide subunits: fragment A known as light chain (50,000 MW or 50 kDa) and fragment B known as heavy chain (100,000 MW or 100 kDa); and both are joined together by a disulphide bond. Normally, the tetanospasmin is cleaved extracellularly by a bacterial protease into fragments A and B.
PATHOGENESIS OF CLOSTRIDIUM TETANI INFECTION
Endospores of C. tetani are introduced into the body through burns, surgical sutures, wounds or invasive injury on the skin; and thus C. tetani only infect humans by chance via wound or injury on the skin. C. tetani is usually a non-invasive pathogen and only cause disease (tetanus) through the action of its exotoxin (tetanospasmin). Tetanospasmin is produced when C. tetani endospores and vegetative cells germinate under the anaerobic conditions created in the wound. The presence of a low oxidation-reduction potential which creates a strict anaerobic environment at the wound site is the main predisposing factor for tetanus in humans.
Usually, the pathogen C. tetani only multiplies locally at the wound site without spreading or causing any significant damage to neighboring tissues but as the injury site becomes anoxic, it grows to produce the tetanus toxin (tetanospasmin) which is carried to the central nervous system (CNS) where it impacts the spinal cord and brain to cause series of unrestrained muscular stimulations. Tetanospasmin (tetanus toxin) binds to gangliosides in synaptic membranes of CNS where it inhibits and suppress the release of inhibitory neurotransmitters (e.g. glycine and gamma-amino butyric acid, GABA), thus causing muscle spasm in key muscular/skeletal sites of the affected individual’s body. The blockage of the release of inhibitory neurotransmitters such as glycine and gamma-amino butyric acid (GABA) leads to convulsive contractions of voluntary muscles in the affected human or animal host.
Generally, this leads to difficulty in swallowing, increased muscle tone, lock jaw/trismus (difficulty in opening the mouth) and rigidity of the muscles (Figure 1). The incubation period of tetanus is variable and often shorter spanning day or weeks after the initial introduction of C. tetani spores into wound sites on the body. Clinical symptoms of tetanus may include trismus or lockjaw (i.e. inability to open the mouth properly), and this may later progress to spasm or muscular contractions in other sites of the body such as the pharyngeal muscles (which affects swallowing).

Risus sardonicus (i.e. spasm of the facial muscles) and opisthotonos (i.e. backward contraction of the back towards the heels) are other complications of the disease. Spasm of the respiratory muscles results in respiratory failures; and this may cause death. Tetanus is a disease with a high mortality rate. In some parts of the world such as Asia and Africa, neonatal tetanus can ensue from failure of observing aseptic technique during childbirth such as when contaminated instruments are used to cut the umbilical cord of the foetus after delivery.
Neonatal tetanus can also occur from improperly or non-immune mothers; and in such situation, the child has not acquired passive immunity from the mother and the umbilical cord can become infected in the process of birth. Female circumcision, unskilled abortion and performing surgery with contaminated or unsterile instruments are other predisposing factor that may cause tetanus in some developing countries.
LABORATORY DIAGNOSIS OF CLOSTRIDIUM TETANI INFECTION
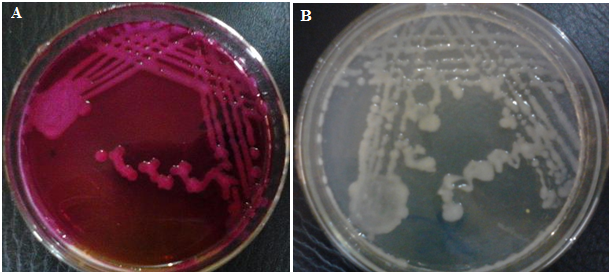
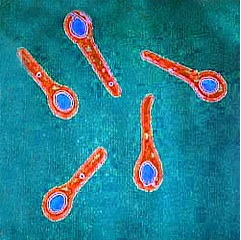
There is rarely any routine laboratory test for the diagnosis of tetanus. However, the clinical diagnosis of the disease in most cases lies on the history of the wound infection and clinical symptoms of the disease (e.g. muscle stiffness) in the individual. Gram staining shows the presence of bacilli with terminal spores that resembles a tennis racket (Figure 2). Examination of blood or tissue for the presence of tetanospasmin is rarely performed but culture can be carried out on selective media to isolate the organism. C. tetani is indole positive.
IMMUNITY TO CLOSTRIDIUM TETANI INFECTION
Prior infection with C. tetani does not confer on the tetanus-patient any form of protection against a possible future infection. Thus, prophylactic vaccination using tetanus toxoid should be administered to newborns in their first year of life, and booster doses given subsequently.
TREATMENT OF CLOSTRIDIUM TETANI INFECTION
Treatment of tetanus should be perfumed without delay using anticonvulsive drugs and regimens that prevent spasm. Tetanus toxin should be neutralized in the affected individual via the administration of antitoxin such as the human tetanus immune globulin, HTIG (human antitoxin).
Wound infections especially those contaminated with soil should be properly taken care of by dressing and the administration of antibiotics such as penicillin which inhibits the growth of C. tetani and toxin production. Sedatives such as benzodiazepines should be given to patients already experiencing muscle spasm; and they should be placed in a quiet dark location and given respiratory support to maintain sufficient airflow in the airway system.
PREVENTION AND CONTROL
Tetanus is a preventable disease. It can be prevented through the use of immunization or vaccination of susceptible human hosts with tetanus toxoid vaccine. C. tetani vaccine contains tetanus toxoid, and the vaccine is administered early in life to neonates or infants and then later in life as booster doses (and for prophylactic immunization) to protect the individual against tetanus infection. Since the treatment of tetanus is often not reliable in some cases, it is advisable that people get active vaccination against the disease using tetanus toxoid vaccines.
C. tetani vaccine known as tetanus toxoid vaccine is usually given as a preventive measure very early in life and in booster doses later in life for protection against the pathogen. Booster doses of tetanus toxoid vaccine should be injected or administered to persons who sustain wound injury of any kind even after stepping on corroded nails or metals. Such measure helps to prevent tetanus in a population. Massive and sustained active immunization against tetanus (though short-lived) is necessary in preventing tetanus in children of developing countries where the mortality rate of the disease is high.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
Discover more from Microbiology Class
Subscribe to get the latest posts sent to your email.